1. Background
Celiac disease (CD) is an autoimmune disorder characterized by small intestinal enteropathy and atrophy of intestinal villi. It occurs in individuals with a genetic predisposition and is triggered by dietary gluten (1, 2). Estimates indicate that CD affects approximately 1% of the world’s population. Its prevalence is reported to be 1.4% based on positive serological tests and 0.7% based on biopsy results (3). The prevalence of CD varies by sex, age, and geographical location. Specifically, the prevalence of CD is 0.4% in South America, 0.5% in Africa and North America, 0.6% in Asia, and 0.8% in Europe and Oceania (4). However, in certain countries such as India and Iran, the prevalence of CD is higher, largely due to the substantial consumption of wheat (4). In studies conducted in Iran, the prevalence of CD was found to be 2% based on duodenal biopsy and 3% based on serological tests, both of which are higher than the global average (5).
Evidence indicates that patients with CD are more prone to other immune-mediated disorders, leading to extra-intestinal manifestations compared to the general population (6, 7). This susceptibility is attributed to the extension of adaptive immune responses beyond intestinal tissues (8). Celiac disease is closely associated with various skin disorders, resulting in dermatological issues, including dermatitis herpetiformis (DH), psoriasis, urticaria, chronic dry skin, erythema nodosum, vitiligo, among others (9). Among these, DH and psoriasis appear to be more closely related to CD. Dermatitis herpetiformis is polymorphic, characterized by lesions that manifest as erythema, plaque, and papule on the head, face, neck, as well as the extensor surfaces of the knees, elbows, shoulders, and sacral region. Psoriasis is identified by red and dry scaly patches on the skin (9).
Although the relationship between DH and CD is well-known, other cutaneous manifestations have been poorly studied. Additionally, CD is often underdiagnosed because the classic signs and symptoms are not present in all patients. Therefore, investigating other extra-intestinal manifestations of CD can lead to a better understanding of the condition.
2. Objectives
In this study, we aimed to assess the presence of skin manifestations in children with CD.
3. Methods
This cross-sectional study was conducted at the Celiac Registry Center, Golestan Research Center of Gastroenterology and Hepatology in Gorgan, northeast Iran, between April and July 2023. The Ethics Committee of Golestan University of Medical Sciences approved the study protocol (IR.GOUMS.REC.1402.481). Written informed consent was obtained from all patients and their parents. Registered patients were invited to participate in the study via phone call (N = 79). Among them, 39 children attended the clinic for evaluation. Inclusion criteria included a CD diagnosis confirmed by positive serology or biopsy and age below 18 years.
A full body examination was conducted by a dermatologist attending the research center as scheduled. The examination included the body, hair, and nails of the patients to detect any cutaneous manifestations. In the case of finding any lesions, patients were assessed and treated according to standard protocols by the dermatologist. Dermatologists classified the findings based on the type, location (face, limbs, head, trunk, and lumbosacral region), duration (acute, chronic, and recurrent), and distribution (symmetric or asymmetric) of the lesions.
The demographic information of patients, details of physical examinations, first anti-tissue transglutaminase antibody (anti-tTg Ab) test results, intestinal biopsy results, and other data were recorded. All data were then analyzed using SPSS version 26 to show central and distributive indices. Quantitative data were reported as mean (standard deviation), and categorical data were reported as number and percent.
4. Results
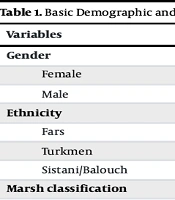
The mean [standard deviation (SD)] age of the patients was 9.84 (4.41) years. The mean (SD) duration of the disease and initiation of the gluten-free diet (GFD) was 4.24 (2.64) years. Five children had a positive family history of CD. The mean (SD) level of anti-tTg Ab in patients was 185.67 (161.79 IU/mL) at the time of CD diagnosis. Histopathology data were available for 31 patients, with Marsh 3b (45.2%) reported as the most common type. The clinical data of the patients are summarized in Table 1.
| Variables | Values a |
|---|---|
| Gender | |
| Female | 21 (53.8) |
| Male | 18 (46.2) |
| Ethnicity | |
| Fars | 17 (44.7) |
| Turkmen | 11 (28.9) |
| Sistani/Balouch | 10 (26.3) |
| Marsh classification | |
| 1 | 1 (3.2) |
| 2 | 3 (9.7) |
| 3a | 8 (25.8) |
| 3b | 14 (45.2) |
| 3c | 5 (12.8) |
| Age (y) | 9.84 ± 4.41 |
| Disease duration (y) | 4.23 ± 2.64 |
| Anti-tTg Ab level (IU/mL) | 185.67 ± 161.79 |
Basic Demographic and Clinical Data of Children with Celiac Disease
Cutaneous manifestations were found in 37 patients (51.3% female). Most of the children (96.4%) experienced chronic skin problems. The distribution of lesions was symmetric in 15.6% of the patients. The most commonly involved areas were the face (16.8%) and limbs (14.4%). Overall, 83 cutaneous lesions were detected. The most common types were dry skin (20.4%), pityriasis alba (15.6%), keratosis pilaris (12%), and pigmentation (10.8%). The details of dermatologic findings are presented in Table 2.
| Dermatological Findings | No. (%) |
|---|---|
| Duration | |
| Acute | 1 (2.6) |
| Chronic | 36 (92.3) |
| Recurrent | 2 (5.1) |
| Distribution | |
| Symmetric | 13 (33.3) |
| Asymmetric | 26 (66.7) |
| Location | |
| Face | 14 (16.8) |
| Trunk | 7 (8.4) |
| Limbs | 12 (14.4) |
| Scalp | 5 (6) |
| Lumbosacral region | 4 (4.8) |
| Nail | 5 (6) |
| Oral cavity | 8 (9.6) |
| Hair | 6 (7.2) |
| Type | |
| Pityriasis alba | 13 (15.6) |
| Dry skin | 17(20.4) |
| Keratosis pilaris | 10 (12) |
| Acne | 5 (6) |
| Hirsutism | 2 (2.4) |
| Seborrheic dermatitis | 5 (6) |
| Pigmentation | 9 (10.8) |
| Nevus | 2 (2.4) |
| Scar | 1 (1.2) |
| Freckle | 1 (1.2) |
| Food allergy | 1 (1.2) |
| Alopecia | 2 (2.4) |
| Allergic contact dermatitis | 1 (1.2) |
| Vitiligo | 1 (1.2) |
| Oral aphthous | 8 (9.6) |
| Paronychia | 2 (2.4) |
| Brittle nail | 2 (2.4) |
| Periungual hyperpigmentation | 1 (1.2) |
Dermatological Findings in Children with Celiac Disease According to the Duration, Distribution, Location, and Types
Among all the patients, 25 cases had at least two findings. Of these, the most common combinations were pityriasis alba with dry skin (9 patients) and dry skin with pigmentation (5 patients).
5. Discussion
Cutaneous manifestations are commonly observed in both pediatric and adult patients with CD (10). In this study, 94.8% of the CD patients experienced at least one mucocutaneous disorder. The skin diseases associated with CD are categorized into five groups (8). The first group includes allergic skin diseases, such as urticaria, chronic urticaria, and atopic dermatitis, which have been related to CD. The second group consists of inflammatory disorders, including pityriasis rubra pilaris, erythroderma, pityriasis lichenoides, and erythema nodosum, which are also found in CD patients. The third group encompasses immune-mediated skin diseases, such as psoriasis, that are associated with CD. Autoimmune disorders, including alopecia areata, cutaneous vasculitis, vitiligo, and lupus erythematosus, are more common in these patients. Lastly, the miscellaneous group includes conditions such as aphthous stomatitis and rosacea, which have also been found to be associated with CD.
In our study, inflammatory skin disorders were the most common type of cutaneous findings, which differs from previous investigations. A cohort study conducted in Sweden collected data from 43,300 CD patients over 45 years and reported an increased risk of eczema, psoriasis, urticaria, vitiligo, and alopecia areata (11). A systematic review and meta-analysis in 2016 showed that the primary cutaneous complications in CD patients included DH, alopecia areata, dermatomyositis, vitiligo, lupus erythematosus, and psoriasis (12). Additionally, another study in India found atopic dermatitis to be the most common skin disorder among children with CD (13). A study by Quratulain et al. showed that autoimmune skin disorders, including psoriasis, DH, and alopecia areata, were frequently found among the patients (14).
Most of the reported disorders were related to immune system malfunction, including allergic, immune-mediated, and autoimmune mechanisms. Several hypotheses attempt to explain this relationship. One justification for this connection is the shared genetic background and similar environmental triggers between CD and certain skin disorders (15). Another explanation involves the alteration in intestinal barrier permeability, which allows gluten to pass into the bloodstream and triggers an inappropriate immune response (16). Additionally, the release of IgE and other immunoglobulins in the submucosa of the small intestine after gluten exposure can lead to the development of urticaria and atopic dermatitis (17). Furthermore, the production of proinflammatory cytokines such as TNF-α and interferon gamma (IFNγ) has been shown to be related to immune-mediated disorders like psoriasis (18).
There have been investigations with findings similar to those of our study. These studies found that inflammatory skin complications are the most common type of cutaneous disorders in patients with CD. A study conducted by Seyhan et al. reported that xerosis and keratosis pilaris were common findings in children with CD (19). The prevalence of inflammatory disorders in CD can be explained by various mechanisms. Gluten-induced activation of T lymphocytes and the release of proinflammatory cytokines can lead to both local and systemic inflammation (20). Additionally, alteration in intestinal permeability that allows the passage of gluten may provoke the inflammatory process, potentially leading to damage in other tissues throughout the body (16). The high rate of inflammatory skin findings in CD patients may also be the result of continuous gluten exposure, even after the initiation of a GFD. Based on our clinical experience, adherence to a GFD is challenging for most patients in Iran (21). This difficulty arises partly from limited access to gluten-free foods and materials, and partly from insufficient knowledge and understanding among patients about the GFD and how to incorporate it into their daily routines. Given these challenges, the high rate of inflammatory skin problems is not unexpected within the population studied.
Dry skin or xerosis is a common finding in most CD patients, including those in our study. Multiple factors can contribute to xeroderma, such as vitamin deficiencies and systemic diseases that appear to be associated with CD (22). Children with CD often face nutritional challenges and lower intakes of essential nutrients (23). Therefore, this issue can be addressed by providing gluten-free sources or supplements to compensate for deficiencies that may be related to skin problems.
In this study, there were limitations that need to be considered. First, the sample size was limited, and a larger population could be more useful for understanding the cutaneous manifestations in CD patients. Second, we did not assess the anti-tTg level of the patients to investigate its association with skin findings and whether they had exposure to gluten. Additionally, the absence of a control group limits the interpretation of our findings specific to the cutaneous findings of CD.
5.1. Conclusions
Cutaneous complications are prevalent among pediatric CD patients, with dry skin, pityriasis alba, and keratosis pilaris being the most common. These findings highlight the need for systematic dermatological evaluations in CD patients to ensure timely diagnosis and management of skin-related complications. It should be kept in mind that these results may not be generalized to other populations with higher GFD adherence or different cultures or ethnicities.