1. Background
Traumatic brain injury (TBI) refers to brain damage caused by external forces, such as blunt trauma, penetrating objects, or acceleration-deceleration impacts. According to annual statistics, nearly 2.5 million individuals in the United States present to emergency departments with complaints of TBI, with a significant number experiencing decreased levels of consciousness, impaired function, and potentially irreversible complications following trauma and head injury. The TBI is a leading cause of death and disability among young adults worldwide and is implicated in nearly half of all trauma-related fatalities. On the other hand, traumatic brain injuries in children have become a significant public health concern, particularly in developing countries. Recent studies have shown that children under the age of six experience more difficulties in neurocognitive development following head injuries than older children. Hospitalization for TBI is more common among adolescents, and boys require more emergency consultations and hospitalizations than girls (1, 2). The importance of managing patients with decreased levels of consciousness in healthcare facilities is highly emphasized, as early and timely identification of certain clinical conditions in these patients significantly impacts treatment outcomes, and prompt intervention can lead to complete recovery without complications. Accurate assessment and treatment based on that assessment reduce complications and mortality in these patients, while precise and early prediction of potential outcomes facilitates decision-making regarding the allocation of hospital resources. Therefore, there is a need for convenient and accurate methods for initial and ongoing assessment and response to treatment; several tools have been developed for assessing levels of consciousness, the most well-known of which is the Glasgow Coma Scale (GCS) (3).
The GCS is a criterion for assessing the level of consciousness, introduced by Scottish researchers Jennett et al. in 1974. This scale evaluates patients’ eye, verbal, and motor responses separately, assigning a specific score to each, which are then summed to yield a total score ranging from 3 to 15. Depending on the resulting score, patients may need specific treatments. Despite its widespread use, the GCS has limitations, with factors like eye injuries and intubation potentially affecting its accuracy (4, 5). Another scale recognized for assessing the level of consciousness is the Full Outline of UnResponsiveness (FOUR) score. In 2005, Wijdicks et al. developed a new assessment scale called the FOUR score to address some of the shortcomings of the GCS. Some studies have suggested that the FOUR provides greater measurement accuracy compared to the GCS, effectively covering some of its deficiencies. It evaluates eye response, motor response, brainstem reflexes, and breathing, scoring from 0 to 16. The FOUR score is beneficial for assessing intubated patients or those with very low GCS scores (GCS ≤ 4) (6, 7). It has a higher prognostic value for intubated patients in the intensive care unit (ICU). The FOUR criteria were initially designed to assess patients admitted to the ICU, but over time, studies have shown that this scale can also be used to evaluate other patients, including emergency patients (8). The TBI is classified into three categories based on the GCS: Mild (13 - 15), moderate (9 - 12), and severe (≤ 8) (9). According to available studies, findings regarding the severity of TBI and its correlation with prognosis indicate that mild TBI (accounting for 75% of cases of TBI) has significantly fewer acute and long-term clinical and paraclinical outcomes compared to moderate and severe TBI, with the risk of mortality in severe TBI being approximately 30 - 60% (10-12). Additionally, studies have shown that although 17% of patients with mild TBI exhibited abnormal findings on brain CT, only 1% had life-threatening findings. Due to the potential for increasing intracranial hematoma, patients with mild TBI should undergo serial evaluations, such as GCS assessments (13).
2. Objectives
The present study aimed to compare the accuracy of two scales, the GCS and the FOUR scores, in relation to mortality among patients with TBI at Shohada-ye Ashayer Hospital. To date, various studies have been conducted on assessing the measures of consciousness level in patients with TBI; however, there remains uncertainty regarding which scale holds greater value and predictive power for patient mortality. This study was conducted to reassess the GCS and FOUR scores in a different community and hospital setting compared to previous studies, to evaluate the prioritization of using these consciousness assessment scales in such patients, and to determine which scale may be more beneficial under varying conditions.
3. Methods
This study is a cross-sectional descriptive-analytical study aimed at comparing the GCS and the FOUR score in predicting mortality in patients with TBI. Conducted in autumn 2023, the study included individuals who presented to the Emergency Department of Shohada-ye Ashayer Hospital with symptoms of TBI. Those with life-threatening injuries to other organs were excluded. Coordination for data collection was established with emergency medicine and surgery teams, along with necessary training provided. A specific checklist was used for data collection (Appendix 1 in the Supplementary File). In young children under 5 years, a modified GCS was used, recognizing that GCS assessment can be difficult, while the AVPU Scale is often prioritized (Appendix 2 in the Supplementary File). Both the GCS and FOUR criteria were assessed at the earliest opportunity after the patient’s arrival in the emergency department by the researcher or emergency medicine colleagues. Patients admitted to the ICU or hospital ward were monitored until they either recovered, died, or were diagnosed with brain death. Other factors like age and gender, as well as the injury mechanism, were also evaluated for their relevance to patient prognosis.
Based on the findings of similar studies, such as Sadaka et al. (14), the area under the ROC curve (AUC) for the FOUR Scale and the GCS was found to be 0.89 and 0.98, respectively. At a 5% error level and 20% power, the required sample size was determined to be 98 cases using the MedCalc software. Using the PASS software and the formula, the required number of patients for this study was calculated to be 110. In this study, 110 participants who met the inclusion criteria were evaluated, most of whom had sustained a TBI due to an accidental mechanism. Of these, 12 patients were excluded from our study due to severe and distracting injuries to maintain result validity. Ultimately, 98 TBI patients were included in the assessment.
Inclusion criteria included all patients who presented to the hospital with complaints of TBI, while exclusions were made for those with sedative use, drug poisoning, or significant auditory, visual, speech, or motor problems, and life-threatening injuries besides head injuries. Results were derived from appropriate descriptive indices such as frequency and relative frequency percentages for qualitative variables, and mean and standard deviation for quantitative variables. To determine the association between qualitative variables and patient prognosis, the chi-square test or Fisher’s exact test was used, while the correlation between quantitative variables was assessed using the correlation coefficient. For comparing the means of quantitative variables at different prognosis levels, an independent t-test or its non-parametric equivalent was employed. Additionally, the ROC curve was used to identify the optimal cutoff points for predicting outcomes in TBI cases, maximizing sensitivity and specificity with the Youden Index.
4. Results
In this study, a total of 98 patients were examined. Among these individuals, 23 (23.5%) were female and 75 (76.5%) were male. The mechanisms leading to head trauma were accidents (53.8%), falls (24.5%), falling objects and accidental head collisions (13.5%), and assaults (8.1%). The mean age of all participants was 35.43 ± 19.54 years. Eighteen of these individuals died (3 cases of brain death and 15 fatalities); 16 males (87.5%) and 2 females (12.5%) among the deceased (Table 1). The use of the chi-square and Fisher’s test showed no significant association between gender and patient outcomes (P = 0.171) or between mechanisms of injury and mortality (P = 0.175). The pediatric population (under 14 years) in this study comprised 9 patients (9.1% of the total patients), of which 2 cases (22.2% of the pediatric population) resulted in death. The mean age of those who died was 40.56 ± 18.668 years, while the mean age of those who survived was 34.28 ± 19.664 years. There was no significant difference between the average age in the two groups (P = 0.078) (Table 1).
| Variables | Outcome | P-Value | |
|---|---|---|---|
| Survival | Death | ||
| Gender | 0.171 | ||
| Female | 21 (91.3) | 2 (8.7) | |
| Male | 59 (78.7) | 16 (21.3) | |
| Mechanism | 0.175 | ||
| Accident | 42 (79.2) | 11 (20.8) | |
| Fall | 20 (83.3) | 4 (16.7) | |
| Incidental collision of an object with the head | 11 (84.6) | 2 (15.4) | |
| Engagement | 8 (100.0) | 0 (0.0) | |
| Age | 34.28 ± 19.66 | 40.56 ± 18.668 | 0.078 |
Demographic and Clinical Characteristics of Patients with Traumatic Brain Injury by Outcome (Survival Versus Death) a
The mean GCS score in individuals who died was 4.56 ± 1.917, while in individuals who survived, it was 13.66 ± 2.859. In comparison, the mean score of the FOUR score in deceased individuals was 3.56 ± 2.526, whereas in survivors, it was 14.75 ± 2.684. The lowest GCS score recorded in individuals who survived was 3, while the lowest FOUR score in these individuals was 5 (Table 2). Utilizing an independent t-test indicated that there was a statistically significant difference between the mean scores obtained on the GCS and FOUR scores for those who died and those who survived (P < 0.001). The correlation coefficient between the two scores, GCS and FOUR, was found to be 0.983, indicating a very strong positive relationship between these two variables (P < 0.001).
| Prognosis | GCS | FOUR |
|---|---|---|
| Death | ||
| Mean ± SD | 4.56 ± 1.917 | 3.56 ± 2.526 |
| Range | 3 - 9 | 0 - 9 |
| Survival | ||
| Mean ± SD | 13.66 ± 2.859 | 14.75 ± 2.684 |
| Range | 3 - 15 | 5 - 16 |
| P-value | < 0.001 | < 0.001 |
Comparison of the Mean and Standard Deviation of Glasgow Coma Scale and Full Outline of UnResponsiveness Scores in Deceased and Survived Patients
The analysis of the eye response component of the GCS indicated that among the 18 individuals who died, approximately 83.3% received a score of 1, while only 5.6% had a score of 4. Among those who scored 1, 75% died, compared to only 1.5% of individuals who achieved a full score (Table 3). A significant correlation was found between eye response and patient prognosis (P < 0.001). In terms of the verbal response component, analysis showed that 76% of individuals who scored 1 died, while none with a full score died (Table 3). The results indicated a high percentage of the deceased had low scores and a strong correlation between the verbal component and prognosis (P < 0.001). For the motor response component, 1.61% of the individuals who died had a score of 1, whereas 77.5% of those who survived had a perfect score (Table 3). Utilizing Fisher’s test demonstrated a strong significant relationship between the motor component and prognosis.
| Responses and Scores | Survive | Death | P-Value |
|---|---|---|---|
| Eye | < 0.001 | ||
| 1 | 5 (25.0) | 15 (75.0) | |
| 2 | 4 (66.7) | 2 (33.3) | |
| 3 | 5 (100.0) | 0 (0.0) | |
| 4 | 66 (98.5) | 1 (1.5) | |
| Verbal | < 0.001 | ||
| 1 | 5 (23.8) | 16 (76.2) | |
| 2 | 5 (71.4) | 2 (28.6) | |
| 3 | 3 (100.0) | 0 (0.0) | |
| 4 | 5 (100.0) | 0 (0.0) | |
| 5 | 62 (100.0) | 0 (0.0) | |
| Motor | < 0.001 | ||
| 1 | 2 (15.4) | 11 (84.6) | |
| 2 | 0 (0.0) | 1 (100.0) | |
| 3 | 2 (33.3) | 4 (66.7) | |
| 4 | 3 (100.0) | 0 (0.0) | |
| 5 | 11 (84.6) | 2 (15.4) | |
| 6 | 62 (100.0) | 0 (0.0) |
Distribution of Glasgow Coma Scale Subscale Scores (Eye, Verbal, Motor Response) According to Patient Outcomes a
In the examination of the eye response of the FOUR, it was indicated that 83.3% of individuals who died received a score of 0, while 81% of those who survived scored 4, and 75% (15 individuals) of those who received a score of 0 died. Among those who achieved a score of 4, the mortality rate was zero (Table 4); results indicated a strong significant correlation between the eye response component of the FOUR score and the prognosis of the patients (P < 0.001). In the evaluation of the motor response component, 61% of deceased individuals scored 0 and 22.2% received a score of 2. Among those who survived, 2.5% (2 individuals) scored 0, and 0% (0 individuals) scored 1. Among individuals who scored 4, 0% (0 individuals) were associated with mortality. Additionally, approximately 84% (11 individuals) of those who received a score of 0 have died. Of the individuals who survived, 77.5% scored 4 (Table 4). The use of Fisher’s test revealed a strong significant correlation between the motor component of the FOUR score and prognosis (P < 0.001).
| Responses and Scores | Survive | Death | P-Value |
|---|---|---|---|
| Eye | < 0.001 | ||
| 0 | 5 (25.0) | 15 (75.0) | |
| 1 | 4 (66.7) | 2 (33.3) | |
| 2 | 5 (100.0) | 0 (0.0) | |
| 3 | 1 (50.0) | 1 (50.0) | |
| 4 | 65 (100.0) | 0 (0.0) | |
| Motor | < 0.001 | ||
| 0 | 2 (15.4) | 11 (84.6) | |
| 1 | 0 (0.0) | 1 (100.0) | |
| 2 | 5 (55.6) | 4 (44.4) | |
| 3 | 11 (84.6) | 2 (15.4) | |
| 4 | 62 (100.0) | 0 (0.0) | |
| Brainstem | < 0.001 | ||
| 0 | 0 (0.0) | 3 (100.0) | |
| 1 | 0 (0.0) | 7 (100.0) | |
| 2 | 1 (16.7) | 5 (83.3) | |
| 3 | 2 (40.0) | 3 (60.0) | |
| 4 | 77 (100.0) | 0 (0.0) | |
| Respiratory | < 0.001 | ||
| 0 | 1 (25.0) | 3 (75.0) | |
| 1 | 4 (25.0) | 12 (75.0) | |
| 2 | 4 (57.1) | 3 (42.9) | |
| 3 | 1 (100.0) | 0 (0.0) | |
| 4 | 70 (100.0) | 0 (0.0) |
Distribution of Full Outline of UnResponsiveness Score Components (Eye Response, Motor Response, Brainstem Reflexes, Respiratory Pattern) by Patient Outcomes a
In terms of brainstem reflexes, among the individuals who died, 16.7% received a score of 0, 33.33% received a score of 1, and 0% received a score of 4 (Table 4). The use of Fisher’s exact test indicated a significant relationship between brainstem reflexes and prognosis (P < 0.001). The respiratory response analysis indicated a similar trend, with a strong correlation between low scores and mortality (Table 4). The use of Fisher’s test indicated a strong correlation between the respiratory response component of the FOUR criteria and patient prognosis (P < 0.001).
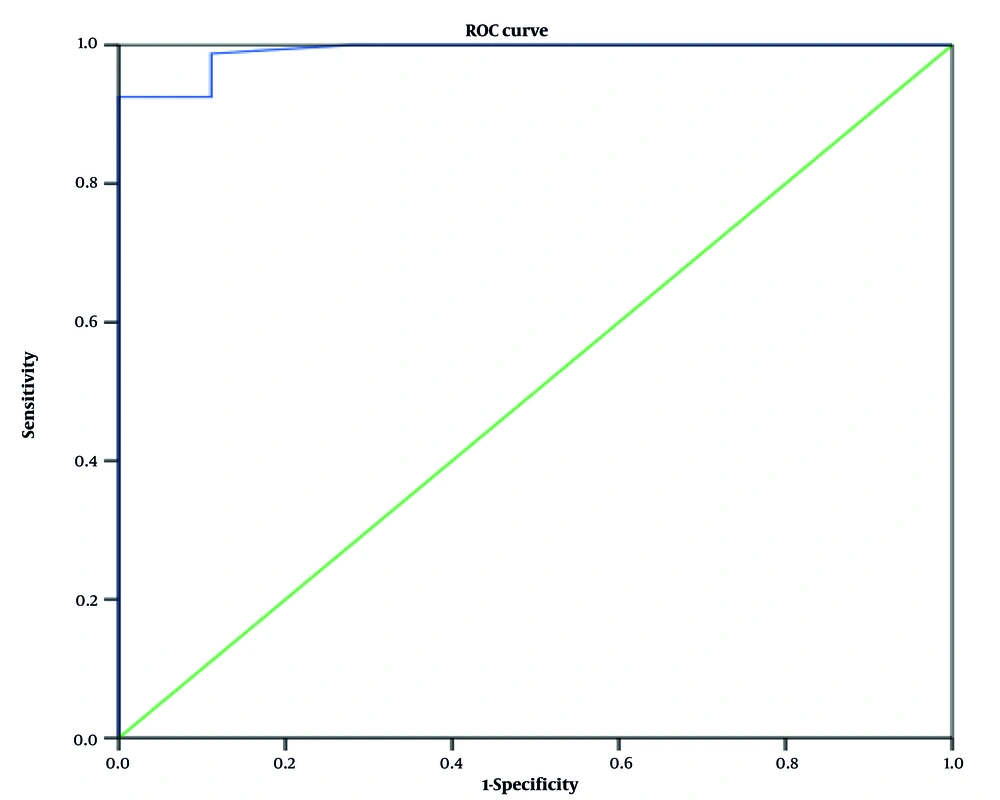
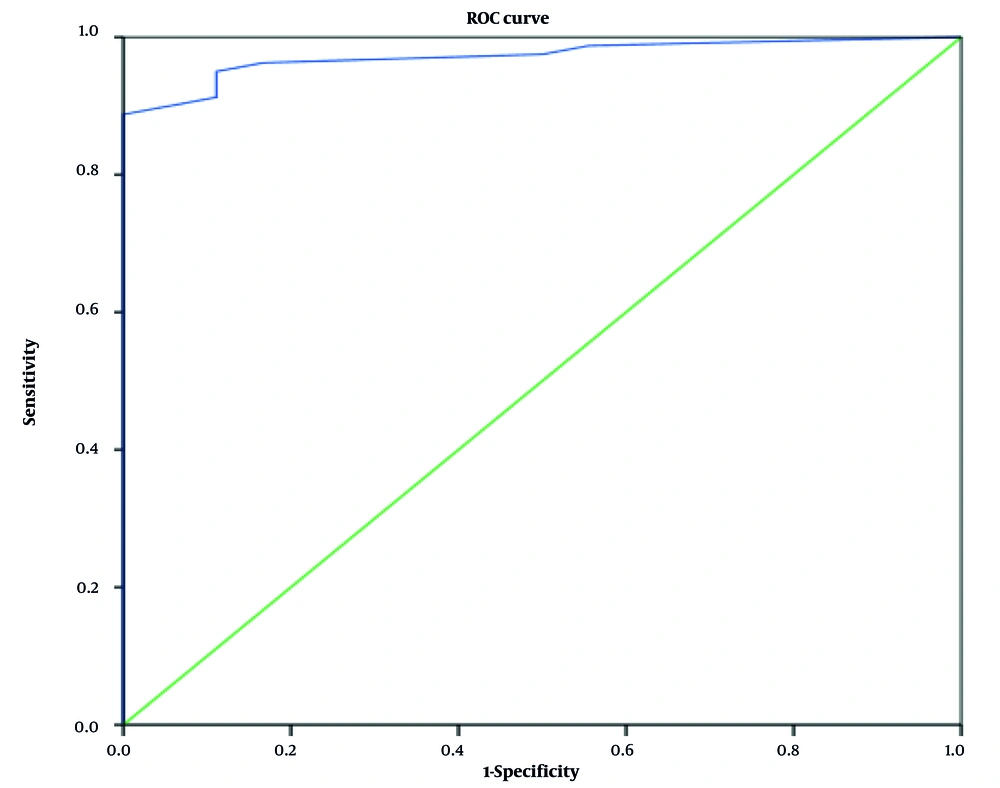
The study classified TBI as mild (65.3%), moderate (11.2%), and severe (23.4%), finding no deaths among mild TBI patients and high mortality rates among those with moderate and severe TBI, emphasizing the importance of TBI severity classification. The AUC for the GCS score in predicting death was obtained as 0.972, indicating that our test (GCS) has a very high ability to predict mortality compared to those who survive (P < 0.001). To determine the optimal cutoff, we are faced with an index known as the Youden Index. Based on this index, our optimal and desirable cutoff point is the one that maximizes the sum of sensitivity and specificity (Figure 1). The ROC curve for the FOUR score had an area of 0.991, leading to a cutoff value of 6 (Figure 2). These findings suggest that patients with scores below these cutoffs have a higher likelihood of mortality. Based on the results, the sensitivity and specificity of the GCS score are 0.950 and 0.889, respectively, and the positive predictive value (PPV) and negative predictive value (NPV) are 0.80 and 0.95, respectively. For the FOUR method, the sensitivity and specificity are 0.988 and 0.889, respectively, and the PPV and NPV are 0.941 and 0.975, respectively.
5. Discussion
The difference in the average age between the two groups of individuals who died and those who survived is approximately 6 years, which may indicate a correlation between increasing age and higher mortality rates among patients. However, this finding is not very reliable due to the broad age range of the patients. In terms of mechanisms, the primary cause of head trauma was accidents, making up 51.8% of cases, whereas studies conducted in the United States, such as McNett et al.’s (13) study, reported falls as the leading cause at 47% of cases. In this study, falls were the second most common cause of TBI at 24.5%. A similar study conducted by Nazari et al. within the country also identified accidents and falls as the most common factors. The most common type of accident was vehicle collisions, which accounted for 20.4% of mechanisms (15). Accidents contributed to 20.8% of deaths among all accident victims, with falls causing 16.6% and impacts with objects accounting for 15.3% (13). In the study by Jamali et al. at Namazi Hospital in Shiraz, the most common cause of death in children with TBI was accidents (69.8%), and a significant correlation was observed between the severity of the injury and the duration of hospitalization (P < 0.001) (2). However, the results indicated no significant correlation between the type of accident and patient outcomes, implying that the accident mechanism is not a crucial risk factor for mortality.
Reviewing past literature reveals scattered results regarding the impact of these two criteria on patient prognosis. Studies such as those by Sadaka et al., Saika et al., and Ahmadi et al. demonstrated that both criteria have shown very similar and acceptable performance in predicting patient prognosis (7, 14, 16). Conversely, studies like that of Okasha et al., Amin et al., and Sekhon et al. have evaluated the performance of the FOUR score as somewhat superior to that of the GCS regarding mortality prognosis, particularly in assessing intubated patients with low GCS and FOUR scores (17-19). Other studies, such as Agrawal et al., found that the GCS score performed better than the FOUR score in predicting outcomes in patients with moderate and mild TBI. The results indicated a significant and precise correlation between the two scales and patient prognosis (P < 0.001). The correlation coefficient was 0.983, indicating a strong relationship, with AUC values for GCS at 0.972 and FOUR at 0.991, showcasing high accuracy for both scales in predicting patient mortality (20). This figure was reported as 0.90 in the McNett et al.’s study (evaluating patients 72 hours after admission) (13). The AUC for differential diagnosis in the studies by Sadaka et al., Saika et al., and McNett et al. (7, 13, 14) for the GCS and FOUR scores respectively, were reported as 0.89 and 0.93, 0.91 and 0.93, 0.93 and 0.91, indicating high accuracy for both scales across all studies. Additionally, based on this curve, cutoff points were also established; a GCS score below 7 and a FOUR score below 6 were associated with high sensitivity and specificity in predicting mortality. However, higher cutoff points resulted in lower predictive capability for mortality (Figures 1 and 2).
In individual evaluation of GCS components, scores in the motor response category were notably linked to mortality, with a score of 1 associated with an 84.61% death rate. The motor response scores 2 and 3 had mortality rates of 100% and 66.66%. The motor component was deemed more reliable compared to other components like verbal and eye response, aligning with findings from previous studies such as the study by Bouakam et al., Okasha et al., and Nyam et al. (17, 21, 22). However, the other GCS components also showed strong predictive accuracy for mortality. Additionally, a high score in these components was associated with a very good prognosis. Among those who survived, 65 patients (81.3%) had a full score on the eye response component, and 62 patients (77.5%) reported a full score on the motor and verbal components. This finding suggests a strong correlation between high scores and survival, backed by significant statistical relevance in their predictive power. Fisher’s test showed that each of the components of the GCS had a significant and precise relationship with patient prognosis when evaluated separately (P < 0.001).
In the evaluation of the components of the FOUR score, the brainstem reflex demonstrated the highest accuracy in predicting mortality, with a score of 0 linked to a 100% death rate, although few individuals were represented. Other data indicated high mortality rates for scores of 0 in the motor, respiratory, and eye response components as well. Full scores in these components were consistently tied to good prognosis, with the brainstem reflex exhibiting the best prognostic strength. It can be concluded that the brainstem reflex component of the FOUR score exhibits the highest accuracy among its components in predicting both mortality and survival. This finding is consistent with studies such as the one by Neyam et al., which identified the brainstem reflex as the strongest component of the FOUR score in prognostic prediction (P < 0.001). However, it contrasts with findings from the study by Buyukcam et al., which reported the highest predictive accuracy related to motor response (AUC = 0.961). The Fisher’s test demonstrated that each component of the FOUR score has a significant and precise correlation with patient prognosis individually (P < 0.001) (17, 21, 22).
5.1. Conclusions
The study demonstrated that both GCS and FOUR scores are effective in predicting mortality in TBI patients, with both scores showing strong correlations and distinct cutoff points for critical assessment. No significant differences were observed in predicting patient prognosis in our study.