1. Background
Chronic kidney disease is recognized as a global public health issue that has garnered significant attention in medicine due to its increasing prevalence, with a tenfold increase in incidence over the last 20 years in the United States. Aghighi et al. reported a 130% increase in the number of patients with end-stage renal disease (ESRD) in Iran from 1997 to 2006 (1). Hemodialysis is the most common treatment method for ESRD, performed through a fistula or permanent or temporary catheters. Although advancements in patient care and dialysis technology have increased the life expectancy of dialysis patients, many still pass away within five years of treatment initiation (1). Mortality rates for these patients are considerably higher than those of the general population.
Malnutrition-inflammation-atherosclerosis (MIA) syndrome is highly prevalent in ESRD patients and is a major contributor to morbidity and mortality. The connection between malnutrition and inflammation drives atherosclerosis, increasing the risk of cardiovascular disease, the leading cause of death in this population. Despite extensive research on MIA syndrome, few studies have examined the role of vascular access types in its development (2). The MIA syndrome represents the interplay between malnutrition, systemic inflammation, and accelerated atherosclerosis, which together contribute to cardiovascular disease, the primary cause of death among dialysis patients.
Malnutrition, a key component of MIA syndrome, is associated with hypoalbuminemia, reduced Body Mass Index (BMI), and impaired immune function, worsening patient outcomes. Inflammation in ESRD patients, characterized by elevated levels of markers such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and white blood cell (WBC) count, is triggered by factors such as uremia, oxidative stress, and frequent vascular access infections. Atherosclerosis, the third component of MIA syndrome, manifests as subclinical vascular changes, such as increased carotid intima-media thickness (CIMT), lipid abnormalities, and the presence of atherosclerotic plaques, collectively increasing the risk of cardiovascular events (3, 4).
Given that vascular access can serve as both a source of inflammation and a potential modifier of nutritional and atherosclerotic parameters, understanding its role in the development of MIA syndrome is crucial for optimizing patient management.
2. Objectives
The present study aims to address this gap by comparing the parameters of MIA in hemodialysis patients using arteriovenous fistula (AVF) and permcath, providing insights into the clinical significance of vascular access in the pathogenesis of MIA syndrome.
3. Methods
3.1. Study Design
This cross-sectional study was conducted from June to August 2022 in two referral educational hospitals, Shafa and Davazdah Farvardin, located in Kerman and Kahnouj cities, Southeast Iran. Patients were selected using a convenience sampling method from the population of hemodialysis patients treated at these centers. The sample size for this study was determined based on the exploratory nature of the research and the available patient population during the recruitment period. The study included 40 hemodialysis patients, divided into two groups based on their vascular access type: Twenty using a permanent catheter (permcath) and 20 using an AVF. While no formal sample size calculation was performed, we ensured that the number of participants was sufficient for detecting clinically relevant differences in MIA parameters between the two groups.
Although no formal matching was performed, demographic and clinical variables (age, sex, primary kidney disease, dialysis duration, smoking, drug use, diabetes, and hypertension) were collected to assess comparability between the groups. Statistical analysis confirmed no significant differences in these characteristics, minimizing confounding effects. However, unmeasured confounders, such as dietary habits and physical activity, may still exist. Demographic variables (age, sex) and clinical variables (primary kidney disease, duration of dialysis, history of smoking, drug use, and comorbidities such as diabetes and hypertension) were collected for all participants using a structured data collection form.
3.2. Exclusion and Inclusion Criteria
3.2.1. Inclusion Criteria
- Adult patients (≥ 18 years) diagnosed with ESRD.
- Undergoing hemodialysis for a minimum of six months.
- Using either a permcath or an AVF as the sole vascular access during this period.
3.2.2. Exclusion Criteria
- Recent hospitalization (within the last three months).
- Fever (axillary temperature > 37.5°C).
- Acute or chronic infectious diseases, including tuberculosis.
- History of coronary artery catheterization, congenital heart disease, or rheumatic diseases.
- Malignancies, cirrhosis, autoimmune diseases, or recent trauma.
- Complications related to dialysis, such as catheter infections or fistula stenosis.
- Kidney transplant recipients or recent COVID-19 infection.
3.3. Study Protocol
The parameters measured in this study were selected to assess the three components of MIA syndrome:
(1) Malnutrition: Serum albumin levels (< 3.5 g/dL considered hypoalbuminemia) and BMI, calculated as weight in kilograms divided by height in square meters.
(2) Inflammation: Serum levels of CRP, ESR, WBC count, and ferritin.
(3) Atherosclerosis: Mean-CIMT, presence of atherosclerotic plaques, and lipid profile (serum triglycerides and cholesterol levels).
Two independent radiologists, blinded to the patients’ clinical and biochemical data, performed ultrasound evaluations of the bilateral carotid arteries. CIMT was measured at 0.5 - 1 cm proximal to the internal carotid artery bulb, and the average of both sides was recorded as the mean CIMT. A CIMT > 1 mm was considered indicative of subclinical atherosclerosis. Atherosclerotic plaques were categorized as unilateral or bilateral based on their presence in the carotid arteries.
Demographic and clinical data, including primary kidney disease, duration of dialysis, smoking history, and use of antihypertensive or diabetes medications, were collected using a structured data collection form. The duration of hemodialysis was recorded in months and compared between the two groups (permcath and fistula) to ensure no significant differences might confound the results. Despite these efforts, we acknowledge that unmeasured confounders, such as physical activity levels, dietary patterns, and socioeconomic factors, may have influenced the results. Laboratory tests for CRP, ESR, and ferritin were performed using standardized kits approved by the Ministry of Health.
3.4. Statistical Analysis
The collected data were analyzed using SPSS version 26 (IBM Corporation, Armonk, NY, USA). Continuous variables, such as BMI, serum albumin levels, ferritin, and CIMT, were expressed as mean ± standard deviation (SD), while categorical variables, such as the presence of hypoalbuminemia, elevated CIMT, or atherosclerotic plaques, were presented as percentages. Continuous variables were tested for normality using the Shapiro-Wilk test. Independent t-tests were applied to normally distributed variables (e.g., albumin, BMI), while non-normally distributed variables (e.g., ESR, ferritin) were analyzed using Mann-Whitney U tests. Categorical variables (e.g., presence of hypoalbuminemia, high CIMT) were compared using chi-square or Fisher’s exact tests. No formal correction for multiple comparisons was performed, but the number of comparisons was kept moderate to reduce the risk of type I errors. Key statistical analyses were independently verified by two statisticians to ensure robustness.
3.5. Minimizing Bias in Study Design and Analysis
Efforts were made to minimize bias during the study design, recruitment, data collection, and analysis phases. Patients were selected consecutively using a convenience sampling method to reduce selection bias, and demographic and clinical variables were collected to ensure comparability between the groups. Laboratory tests were conducted using standardized methods, and ultrasound assessments were performed by two blinded radiologists to minimize measurement bias. Data collection followed a standardized protocol, and all data were anonymized before analysis to reduce observer bias. Despite these efforts, residual bias from unmeasured confounders, such as dietary habits and socioeconomic factors, cannot be excluded.
3.6. Ethical Approval
This study was conducted in full compliance with the principles of the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Kerman University of Medical Sciences. Written informed consent was obtained from all participants prior to the initiation of the study. All data were anonymized, and no identifiable information was included in the analysis or manuscript to ensure patient privacy and confidentiality.
4. Results
The demographic and clinical characteristics of the two groups were as follows: Most patients (55%) were women, and the majority were between 45 and 65 years old. Diabetes mellitus and hypertension were the most common primary kidney diseases in both groups. Specifically, 55% of the fistula group and 60% of the permcath group were diabetic, while 85% of the fistula group and 70% of the permcath group were hypertensive, showing no statistically significant difference between the groups (P ≥ 0.05). Similarly, 5% of patients in the fistula group and 20% of patients in the permcath group were smokers, while 20% of patients in both groups were opium users, with no significant differences observed. The mean duration of hemodialysis was 28.5 ± 6.2 months in the permcath group and 30.1 ± 5.8 months in the fistula group. Statistical analysis using an independent t-test showed no significant difference in the duration of hemodialysis between the two groups (P ≥ 0.05). These findings indicate that the two groups were comparable in terms of demographic and clinical variables, supporting the validity of the subsequent comparisons made regarding MIA parameters.
4.1. Malnutrition Parameters
4.1.1. Albumin and Body Mass Index
Among patients with ESRD undergoing hemodialysis, those utilizing fistulas exhibited normal albumin levels in all cases, whereas 80% of patients using permcath also had normal albumin levels. This difference in albumin levels was statistically significant (P = 0.03). The results indicated that 45% of patients undergoing hemodialysis with a fistula and 60% of those using a permcath had BMIs ranging from 5.18 to 99.24. However, this difference was not statistically significant (P ≥ 0.05).
4.2. Inflammation Parameters
4.2.1. White Blood Cell
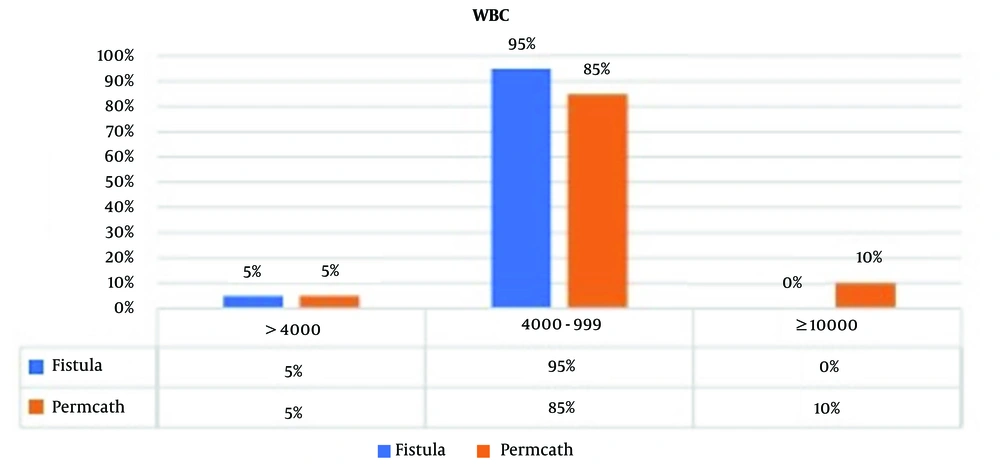
Among ESRD patients undergoing hemodialysis with a fistula, 5% had WBC counts ≤ 3999 cells/μL, and no cases of WBC counts ≥ 10,000 cells/μL were observed. In contrast, among patients using a permcath, 5% had WBC counts ≤ 3999 cells/μL, 85% had WBC counts between 4000 and 9999 cells/μL, and 10% had WBC counts ≥ 10,000 cells/μL. This difference was not statistically significant (P ≥ 0.05) (Figure 1).
4.2.2. Erythrocyte Sedimentation Rate and CRP
Seventy percent and 90% of patients undergoing dialysis with a fistula and 55% and 75% of those using a permcath had normal ESR and CRP levels, respectively, while the remaining patients exhibited elevated ESR and CRP levels. There was no statistically significant difference between the groups regarding ESR (P ≥ 0.05) and CRP (P ≥ 0.05) (Table 1).
4.2.3. Ferritin
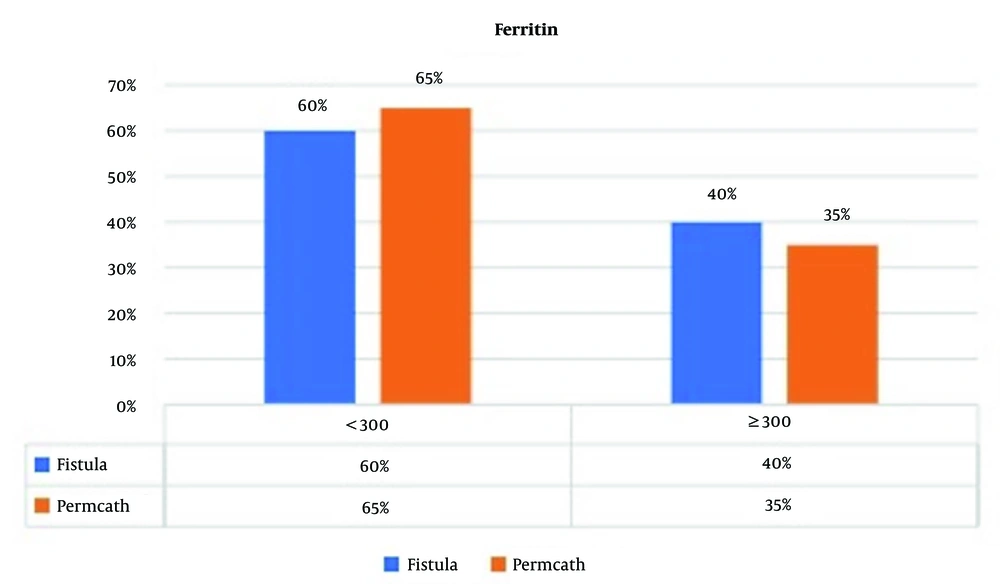
Sixty percent of patients undergoing hemodialysis with a fistula and 65% of those using a permcath had ferritin levels < 300 ng/mL, while the remaining patients had ferritin levels ≥ 300 ng/mL. This difference was not statistically significant (P ≥ 0.05) (Figure 2).
4.3. Atherosclerosis Parameters
4.3.1. Mean-CIMT
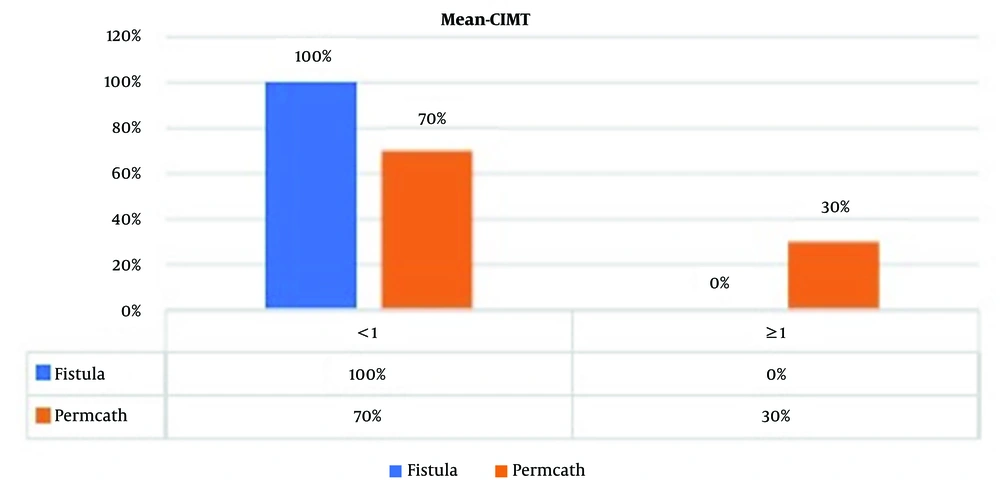
All patients undergoing hemodialysis with a fistula and 70% of those using a permcath had a mean CIMT ≤ 1 mm. This difference was statistically significant (P = 0.008) (Figure 3).
4.3.2. Unilateral and Bilateral Atherosclerotic Plaque
Seventy percent of patients undergoing hemodialysis with a fistula and 65% of those using a permcath had at least one unilateral atherosclerotic plaque, with no statistically significant difference between the groups (P ≥ 0.05). Additionally, 35% of patients undergoing hemodialysis with a fistula and 55% of those using a permcath had bilateral atherosclerotic plaques, which also showed no significant difference (P ≥ 0.05) (Table 2).
4.3.3. Lipid Profile
4.3.3.1. Serum Triglyceride and Cholesterol Levels
Eighty-five percent of patients undergoing hemodialysis with a fistula and 80% of those using a permcath had serum triglyceride levels < 200 mg/dL, with no statistically significant difference (P ≥ 0.05). Additionally, 100% of patients undergoing hemodialysis with a fistula and 95% of those using a permcath had serum cholesterol levels < 200 mg/dL, also showing no significant difference (P ≥ 0.05).
5. Discussion
The MIA syndrome is a well-established predictor of morbidity and mortality in hemodialysis patients, with its components—MIA—being interrelated. Our findings highlight significant differences in malnutrition and atherosclerosis parameters between patients using permcath and those using a fistula, suggesting that vascular access may play a role in the development of MIA syndrome. Specifically, none of the patients in the fistula group had hypoalbuminemia (serum albumin < 3.5 g/dL), while 20% of the permcath group exhibited hypoalbuminemia. This difference was statistically significant (P = 0.03). Hypoalbuminemia is a well-established marker of malnutrition and is strongly associated with increased morbidity and mortality in hemodialysis patients. The absence of hypoalbuminemia in the fistula group suggests that fistula use may contribute to improved nutritional status, potentially due to lower rates of infection and inflammation compared to permcath.
In terms of atherosclerosis, all patients in the fistula group had a CIMT ≤ 1 mm, while 30% of patients in the permcath group had a CIMT >1 mm, indicating subclinical atherosclerosis. This difference was statistically significant (P = 0.008). The CIMT is a reliable predictor of cardiovascular disease and mortality, and its elevation in the permcath group highlights the potential role of vascular access in promoting atherosclerotic changes. The higher prevalence of subclinical atherosclerosis in the permcath group may be attributed to the increased risk of systemic inflammation and endothelial dysfunction associated with catheter use.
Several studies have examined the impact of vascular access type on MIA in hemodialysis patients. However, direct comparisons between permcath and fistula use in the context of MIA syndrome remain limited. Our findings align with previous research highlighting the advantages of fistula-based dialysis in reducing malnutrition and atherosclerosis risks. Ravani et al. systematically reviewed the clinical outcomes associated with different vascular access types and found that catheter use was linked to the highest mortality and cardiovascular risk, whereas fistula use was associated with the most favorable outcomes. Our findings reinforce this, demonstrating that the permcath group exhibited significantly higher rates of malnutrition (as indicated by hypoalbuminemia, P = 0.03) and subclinical atherosclerosis (CIMT > 1 mm in 30% of permcath patients, P = 0.008), whereas these complications were absent in the fistula group (5).
Similarly, Chiu et al. found that hypoalbuminemia was more prevalent in patients using permcath, and low albumin levels were strongly associated with increased mortality. These findings align with our observation that none of the fistula group had hypoalbuminemia, while 20% of the permcath group exhibited hypoalbuminemia (P = 0.03). Hypoalbuminemia is a well-recognized marker of malnutrition and inflammation, and its higher prevalence in the permcath group may be attributed to the increased risk of catheter-related infections and systemic inflammation (6).
Elevated CIMT is a reliable predictor of subclinical atherosclerosis and cardiovascular disease. Patel et al. and Ravani et al. similarly reported that catheter use was associated with higher CIMT and an increased risk of cardiovascular events. This aligns with our observation that 30% of the permcath group had a CIMT > 1 mm, whereas none of the patients using a fistula exhibited this finding. The higher prevalence of subclinical atherosclerosis in permcath users may be attributed to chronic inflammation, endothelial dysfunction, and oxidative stress associated with catheter use, factors that have been implicated in vascular disease progression (5, 7).
Among kidney replacement modalities, hemodialysis is a common treatment in Iran and worldwide (8, 9). Although AVF is the most optimal form of vascular access, the late presentation of patients and vascular disorders have led to an increase in the prevalence of permanent hemodialysis catheters for access in patients with ESRD (10). Complications related to these catheters, especially blood infections, contribute to increased mortality and costs (11). Management of MIA syndrome may improve the cardiovascular epidemic and poor outcomes in dialysis patients (12). Several studies have investigated MIA syndrome in patients undergoing peritoneal dialysis and hemodialysis, but none have specifically addressed the role of vascular access in hemodialysis as a possible risk factor (2, 12-15). Considering the increased use of permanent catheters for hemodialysis in recent years, it is necessary to investigate this issue.
We found that all patients undergoing hemodialysis using a fistula had a CIMT ≤ 1 mm, while 30% of patients using a permanent catheter had a mean CIMT > 1 mm, indicating a significant difference between the two groups. The CIMT is a predictor of coronary heart disease and represents subclinical and asymptomatic atherosclerotic vascular diseases (7). Healthy middle-aged adults with CIMT between 0.6 and 0.7 mm are considered normal, whereas a CIMT exceeding 1 mm is associated with a substantial risk of coronary heart disease (16). Various risk factors related to CIMT levels include age (17), systolic and diastolic blood pressure (7), LDL and HDL levels (7, 18-20), blood urea, serum creatinine, hemoglobin levels, history of diabetes (18), and magnesium levels (21). We aimed to compare two similar groups in terms of risk factors to investigate the type of vascular access as a possible risk factor for increased CIMT. Consistent with our findings, a systematic review showed that individuals using catheters for hemodialysis had the highest risk of death and cardiovascular events compared to patients with other types of vascular access, with patients using fistulas exhibiting the lowest risk (5).
Our findings also revealed that albumin levels were markedly lower in the group using permanent catheters. A study conducted in 2019, which aimed to compare mortality and morbidity between fistula and permanent catheter dialysis patients, also found that albumin levels were lower in the permanent catheter group, with low albumin levels associated with all-cause mortality (6). This study is noteworthy, as the biochemical parameters of MIA syndrome in hemodialysis patients have not yet been documented in Iran. Additionally, it addresses an important gap in understanding which vascular access method is more favorable for patients undergoing hemodialysis. This study revealed that CIMT > 1 mm is more common and albumin levels are lower in the permanent catheter group. However, it had some limitations. Several parameters of MIA syndrome and early atherosclerosis, such as serum homocysteine, lipoprotein (a), physical activity, atherogenic diet, and inflammatory and prothrombotic muscle factors, could not be assessed due to budget constraints and the study design. Additionally, tests were only performed once due to insufficient funding, so studies with larger sample sizes and cohort designs examining all risk factors are suggested.
Central venous catheters, as one type of vascular access, have been well received by hemodialysis patients due to their simplicity of installation and immediate usability. Nevertheless, these forms of vascular access bear the highest rate of complications. We found that CIMT > 1 mm is more common and albumin levels are lower in the permanent catheter group, and both factors increase the risk of mortality due to cardiovascular events. Therefore, in addition to proper self-care training, hemodialysis patients should take appropriate measures to change from a permanent catheter to an AVF, which has fewer complications, as soon as possible.
The significant differences observed in malnutrition and atherosclerosis parameters between the permcath and fistula groups can be explained by several underlying mechanisms:
(1) Malnutrition and hypoalbuminemia: Hypoalbuminemia, a marker of malnutrition, was significantly more prevalent in the permcath group (20%) compared to the fistula group (0%). This finding aligns with previous studies linking permcath use to an increased risk of infection and systemic inflammation, which can lead to poor nutritional status (12). Frequent infections associated with permcath use, such as catheter-related bloodstream infections, trigger a pro-inflammatory state characterized by the release of cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These cytokines promote protein catabolism and reduce albumin synthesis in the liver, leading to hypoalbuminemia. In contrast, AVF use is associated with a lower risk of infections and a more stable systemic inflammatory state, which may protect against malnutrition (14). Additionally, chronic inflammation due to permcath use can impair appetite and nutrient absorption, further exacerbating malnutrition. The absence of hypoalbuminemia in the fistula group suggests that fistula use may help maintain better nutritional balance by minimizing infection-related inflammation and its metabolic consequences (6).
(2) Atherosclerosis and elevated CIMT: The higher prevalence of subclinical atherosclerosis, as indicated by CIMT > 1 mm in the permcath group (30%) compared to none in the fistula group, may be attributed to the pro-inflammatory and pro-atherogenic effects of catheter use. Permcath insertion is associated with chronic endothelial injury and a persistent low-grade inflammatory state, both of which contribute to accelerated atherosclerotic changes (16).
Chronic inflammation can promote endothelial dysfunction, characterized by reduced nitric oxide (NO) bioavailability and increased expression of adhesion molecules, such as vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1). These changes facilitate the recruitment of monocytes and the formation of atherosclerotic plaques. Furthermore, the presence of a catheter in the central venous system may lead to altered hemodynamics and increased shear stress, further contributing to vascular damage (5, 7). Fistula use, on the other hand, is associated with better vascular health due to its reduced risk of infections and lower systemic inflammatory burden. Studies have shown that fistula use is linked to improved endothelial function and greater vascular stability compared to permcath.
(3) Systemic inflammation and its role: Although markers of inflammation (CRP, ESR, WBC, ferritin) did not differ significantly between the two groups in this study, it is important to note that inflammation is a dynamic process, and single-time measurements may not fully capture the chronic inflammatory burden. The higher prevalence of malnutrition and subclinical atherosclerosis in the permcath group likely reflects a cumulative inflammatory burden over time. Permcath use is associated with a higher risk of catheter-related infections, which trigger a persistent inflammatory state (12). Pro-inflammatory cytokines such as IL-6 and TNF-α contribute to protein catabolism and reduced albumin synthesis, leading to hypoalbuminemia (14). Interleukin-6 and TNF-α promote vascular inflammation and endothelial damage, accelerating atherosclerosis progression (15). Additionally, the presence of a central venous catheter causes mechanical irritation and endothelial damage, leading to increased expression of adhesion molecules (VCAM-1, ICAM-1) (13). Inflammatory mediators induce oxidative stress, reducing NO bioavailability, which impairs vasodilation and promotes vascular stiffness (16). These findings support the role of vascular access type as a key determinant of nutritional and cardiovascular outcomes in hemodialysis patients.
(4) Clinical implications of vascular access: The observed differences in malnutrition and atherosclerosis parameters underscore the clinical importance of vascular access type in hemodialysis patients. Permcath use, while convenient and immediately functional, is associated with higher rates of complications, including infections, inflammation, and cardiovascular events. In contrast, fistula use is associated with better long-term outcomes, including improved nutritional status and reduced risk of atherosclerosis. These findings highlight the need to prioritize fistula creation in eligible patients and to implement targeted interventions to mitigate the risks associated with permcath use in patients who are not candidates for fistula (5, 11).
5.1. Conclusions
This study highlights the clinical significance of vascular access type in hemodialysis patients, demonstrating that fistula use is associated with better outcomes in terms of malnutrition and subclinical atherosclerosis compared to permcath. Specifically, the absence of hypoalbuminemia and lower prevalence of elevated CIMT among fistula users underscore its protective role against malnutrition and cardiovascular risks, likely due to reduced infection and inflammation rates. These findings support the prioritization of fistula creation in eligible patients to improve nutritional status, minimize cardiovascular risk, and enhance overall outcomes. However, this study is not without limitations, including its small sample size, cross-sectional design, and the use of single-time measurements for biochemical and clinical parameters. These factors limit the generalizability of the results and the ability to establish causality. Future studies should investigate the long-term effects of vascular access type on cardiovascular outcomes, including mortality, myocardial infarction, and stroke. Additionally, examining inflammatory markers such as IL-6 and TNF-α could provide insights into the role of chronic inflammation in MIA syndrome. Longitudinal studies with larger sample sizes are needed to confirm these findings and establish causality.
5.2. Limitations
This study has several limitations that should be acknowledged. First, the small sample size of 40 patients limits the generalizability of the findings and reduces statistical power for subgroup analyses. Second, the cross-sectional design restricts the ability to establish causal relationships between vascular access type and the observed differences in malnutrition and atherosclerosis. Third, the parameters of MIA were assessed at a single time point, which may not fully capture the chronic and dynamic nature of these processes. Additionally, certain markers of MIA syndrome, such as IL-6, TNF-α, and homocysteine, were not included due to resource constraints. Finally, the study was conducted in a specific geographic region using convenience sampling, which may limit the broader applicability of the results. Future studies with larger cohorts, longitudinal designs, and more comprehensive assessments are recommended to validate and expand upon these findings. This study is also limited by the absence of key inflammatory biomarkers such as IL-6 and TNF-α, which could provide a deeper understanding of inflammation-related malnutrition and atherosclerosis. Additionally, all biochemical and clinical parameters were measured only once, preventing the assessment of dynamic changes over time. Future studies should incorporate longitudinal measurements and additional biomarkers to better characterize the impact of vascular access on MIA syndrome.