1. Background
Infertility represents a significant challenge due to the substantial physical and psychological burden it imposes on affected couples (1). The World Health Organization (WHO) estimates that approximately 10% of women globally experience infertility, contributing to a significant overall burden. While precise data on the prevalence of infertility in Asian and Latin American countries is limited, WHO statistics indicate that the rates among couples of reproductive age in these regions range from 8% to 12% (2). A systematic review conducted in Iran revealed a prevalence of primary infertility at 18.3%, with secondary infertility reported at 2.5%. The causes of primary infertility have been attributed to female factors (32%), male factors (43.3%), both partners (12.5%), and unknown factors (13.6%) (3). The variation in infertility prevalence across countries is influenced by geographical diversity, cultural norms, environmental conditions, socioeconomic factors, and healthcare system evaluations (4). Furthermore, infertility is frequently associated with stigma (5), which may deter couples from seeking treatment or assistance due to anxiety related to this stigma (1). This circumstance can lead to negative emotional states and a diminished quality of life (6). Estimates suggest that approximately 53% to 64% of infertile women worldwide experience stigma (7). This prevalence highlights the necessity for further research.
There is currently no standardized definition of stigma related to infertility. Women experiencing infertility often encounter feelings of guilt, shame, and self-blame following their diagnosis, largely driven by fears of social and familial rejection and embarrassment (8). Some women may be reluctant to engage with community members, resulting in increased social isolation and subsequent depression (5). In 1963, American Sociologist Erving Goffman noted that individuals labeled with "social discrediting" are frequently treated with disregard by others (9). Discussions surrounding infertility often employ derogatory terms, disproportionately affecting couples and women (10). Goffman introduced the concept of stigma in 2009, positing that it can severely impair an individual's social skills and isolate them from positive social interactions, exemplifying a form of public stigma (11). Establishing connections with others, particularly family and friends, can help alleviate mental health issues (12).
In many societies, infertile women grapple with challenges to their primary feminine identity and perceive themselves as less valuable, not only for failing to meet societal expectations regarding reproductive capabilities but also due to diminished self-esteem; consequently, this form of stigma evolves into self-stigma. Childless women frequently experience the negative repercussions of infertility more acutely in developing countries compared to their counterparts in developed nations (13). Individual characteristics of infertile women may correlate with stigma. One study identified factors such as the type and duration of marriage, interactions with others, and the community's emphasis on childbearing as significant predictors of the stigma encountered by infertile women, particularly in countries like Israel (14). Stigma can profoundly affect women's daily activities and employment, significantly hindering the societal participation of infertile women (15). Employment plays a crucial role in shaping perceptions of stigma (16). Women with stable jobs and adequate income typically report better coping mechanisms related to their infertility and experience lower levels of guilt and sensitivity. However, the available information on this subject remains contradictory (17), and it is unclear whether employment directly influences the perception of infertility stigma. Furthermore, existing research is incomplete, underscoring the need to address infertility stigma to enhance interactions with infertile women (18).
Before implementing interventions aimed at improving public interactions, it is essential to understand the predictors of infertility stigma perception. Infertile women, regardless of age, job position, or educational background, encounter various forms of stigma. Empowering these women is critical for alleviating the psychological impact of infertility stigma (19). Healthcare professionals can foster a supportive environment for individuals facing infertility, aiding couples in better understanding the stigma and providing appropriate psychological counseling. This approach can promote a more positive outlook on infertility treatment (20). However, studies examining predictive factors associated with infertility stigma are limited, and existing research is often inconsistent. Fertility holds significant importance in Iranian society, particularly in efforts to increase the young population. Nonetheless, some couples refrain from seeking treatment due to the stigma associated with infertility (1). Therefore, identifying the predictive factors related to the perception of infertility stigma is essential.
2. Objectives
To determine the association between stigma and the demographic and obstetrical characteristics of infertile women.
3. Methods
3.1. Study Design
This study was a cross-sectional analysis conducted at the infertility clinic of Akbarabadi Hospital in Tehran, Iran, from 2021 to 2022. It was developed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (21).
3.2. Sampling Approach
The study focused on 270 infertile women who attended the Infertility Center at Shahid Akbarabadi hospital in Tehran, Iran. A convenience sampling method was employed. The study was conducted from October 2021 to February 2022. Inclusion criteria for participants included a history of primary infertility caused by female, male, or unknown factors; being aged 20 to 45 years; the absence of conditions that could pose life-threatening risks if the women became pregnant; and no diagnosed psychological problems as confirmed by a physician or self-report. Exclusion criteria included incomplete questionnaire responses. We used G*Power software version 3.1.9.2 to determine the sample size, which calculated a required number of 270 participants, with α = 0.05, a power of 0.8, an effect size of 0.03, and consideration of 9 predictor variables.
3.3. Measurements
Two questionnaires were used to collect data on personal information, obstetric history, and infertility stigma. Personal information and obstetric history included women's age, length of marriage, education level, employment status, and economic situation. The obstetric section also covered the duration of infertility, causes of infertility, history of abortion, and any comorbidities such as hypothyroidism, hyperprolactinemia, and obesity. These medical conditions had to be confirmed by a physician or documented in medical histories.
Another instrument used was the Infertility Stigma Scale (ISS) developed by John Li in China. This questionnaire consists of 27 items designed to assess four dimensions of infertility stigma: Low self-worth, societal rejection, social stigma, and family stigma. Each item is rated on a 5-point Likert scale, ranging from complete disagreement (1 point) to complete agreement (5 points), resulting in a total score ranging from 27 to 135. Higher scores indicate greater stigma (22). The scale was validated in Persian by Rajabi et al., who assessed convergent validity using the Self-Criticism Scale, which consists of 22 items. The Pearson correlation test showed a significant relationship between the ISS and the Self-Criticism Scale (r = 0.61, P < 0.001). Reliability was assessed through a test-retest method after two weeks, yielding r = 0.58, P < 0.001. Cronbach's alpha coefficients were 0.95 for total infertility stigma, 0.85 for public stigma, 0.74 for family stigma, 0.91 for social stigma, and 0.90 for self-stigma (23).
Informed written consent was obtained from all participants, who were thoroughly educated about the study's purpose and procedures. Participants were assured that their information would remain confidential. All methods adhered to the study protocol. This study received approval from the Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.REC1395.95-04-28-9311373007).
3.4. Data Analysis
Data were processed and analyzed using Stata version 14. The normality of quantitative variables was assessed using the Shapiro-Wilk test. For non-normally distributed quantitative variables, results were reported as medians and interquartile ranges. Qualitative variables were reported as frequencies and percentages. The Wilcoxon rank-sum (Mann-Whitney) test was applied to variables such as employment status, history of abortion, and underlying disorders. The Kruskal-Wallis test was used for classified variables, including age, duration of marriage, duration of infertility, education level, economic status, and causes of infertility.
Multivariate analysis was conducted to identify factors influencing women's understanding of infertility stigma. We verified the assumptions of the regression model by checking the normality of the residuals, the homogeneity of variance of the residuals concerning the independent variables, the presence of a linear relationship between dependent and independent variables, and the absence of multicollinearity among the independent variables. Consequently, a multiple linear regression model was employed. The assumption of non-collinearity among the independent variables was assessed using the variance inflation factor (VIF) test, which revealed values close to one for all variables. This finding confirmed the appropriateness of using robust multiple linear regression to examine the factors associated with infertility stigma while ensuring the homogeneity of the variance of the residuals relative to the independent variables.
In the multiple linear regression analysis, infertility stigma was treated as a dependent variable in two forms: Once as a standalone measure and again categorized by area. Independent variables included demographic and obstetric factors with a significance level of less than 0.2 in the bivariate analysis. These included employment status, comorbidity, causes of infertility, and economic status, which were incorporated into the model using the Enter method. A significance level of less than 0.05 was considered statistically significant.
4. Results
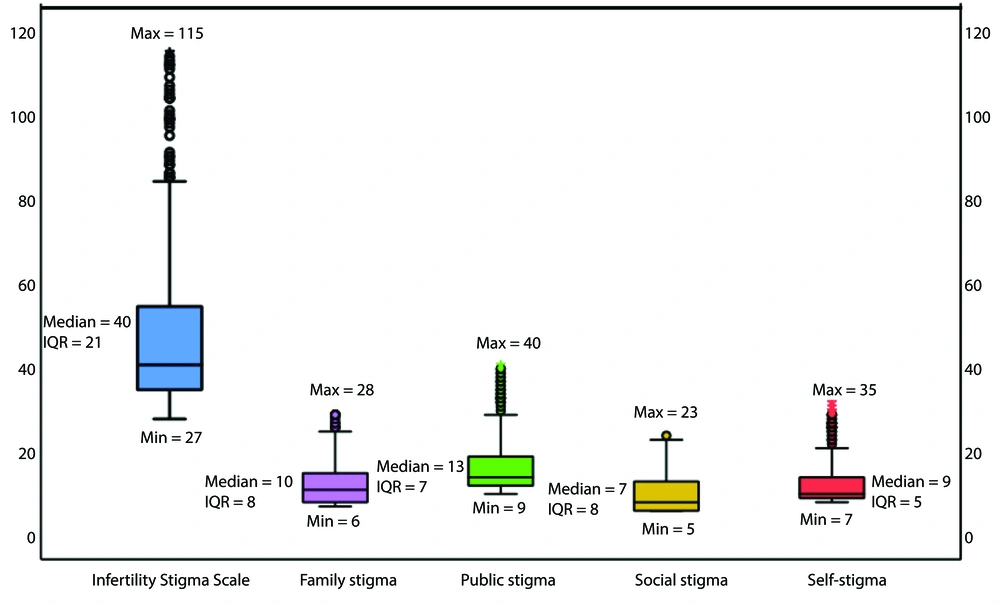
A total of 270 infertile women were included in the analysis. Infertility stigma did not follow a normal distribution. Descriptive statistics for demographic and obstetrical information are presented in Table 1. Among the dimensions of infertility stigma, the social stigma dimension had the lowest median score, while the public stigma dimension had the highest median score. The total score for infertility stigma is presented in Figure 1.
| Variables | No. (%) | Stigma Score; Median (IQR) | P-Value a |
|---|---|---|---|
| Age (y) | 0.18 | ||
| 20 - 25 | 98 (36.3) | 41 (20) | |
| 26 - 30 | 120 (44.5) | 39 (20) | |
| 31 - 35 | 45 (16.6) | 39 (22) | |
| 36 - 40 | 7 (2,6) | 45 (22) | |
| Duration of marriage (y) | 0.47 | ||
| 1 - 5 | 164 (60.7) | 40 (19) | |
| 6 - 10 | 79 (29.3) | 40 (37) | |
| >11 | 27 (10) | 42 (34) | |
| Duration of infertility (y) | 0.54 | ||
| 1 - 5 | 225 (83.3) | 40 (20) | |
| 6 - 10 | 31 (11.5) | 43 (26) | |
| ≤ 11 | 14 (5.2) | 41 (28) | |
| Education level | 0.49 | ||
| Primary school | 4 (1.5) | 41 (28) | |
| Secondary school | 44 (16.3) | 40 (17) | |
| Diploma | 141 (52.2) | 41 (29) | |
| Academy | 81 (30) | 39 (19) | |
| Occupation status | 0.009 b | ||
| Housewife | 178 (65.9) | 42 (26) | |
| Employee | 92 (34.1) | 38 (18) | |
| Economy status | 0.06 c | ||
| Inappropriate | 14 (5.2) | 44 (49) | |
| Relatively appropriate | 210 (77.8) | 41 (24) | |
| Appropriate | 46 (17) | 36 (8) | |
| Reason of infertility | 0.18 | ||
| Male | 2 (0.7) | 40 (20) | |
| Female | 122 (45.2) | 40 (21) | |
| Unknown | 95 (35.2) | 40 (22) | |
| Both | 51 (18.9) | 41 (24) | |
| Recurrent miscarriage history | 0.26 | ||
| Yes | 66 (24.4) | 42 (32) | |
| No | 204 (75.6) | 39 (20) | |
| Underlying disorder d | 0.03 | ||
| Yes | 54 (20) | 44 (48) | |
| No | 216 (80 | 39 (19) |
Association Between Total Infertility Stigma with Demographic and Obstetrical Characteristics in Infertile Women (n = 270)
The results from the Wilcoxon rank-sum test indicated a statistically significant relationship between the stigma of infertility and employment status, as well as a significant correlation with several comorbidities, including hypothyroidism, hyperprolactinemia, and obesity. Using the Kruskal-Wallis test, a weak relationship was found between infertility stigma and economic status. However, no statistically significant relationships were observed between infertility stigma and marriage duration or the length of infertility. The assumption of normal distribution for the residuals was confirmed.
The results indicated that infertile women with favorable economic conditions experienced lower levels of infertility stigma compared to those with unfavorable economic conditions. Specifically, higher economic status correlated with a reduction in the average total score of infertility stigma. A favorable economic level was significantly associated with public infertility stigma and family infertility stigma. Infertile women without comorbidities such as thyroid disorders, elevated prolactin levels, and obesity had a lower mean score in infertility stigma compared to those with these chronic conditions. Women without these disorders exhibited an infertility stigma score significantly lower than those with the disorders. While the presence of these physical disorders was associated with high self-stigma, no statistically significant difference was found for social stigma.
A weak relationship was observed between employment status and the total mean score in infertility stigma. The total mean stigma score was slightly lower among employed infertile women compared to housewives. However, employment status was statistically significantly associated with social infertility stigma, with lower average scores for social stigma among employed women. According to the current results, a portion of the changes (approximately 11%) in infertility stigma were related to independent variables such as employment status, economic conditions, and comorbidities in conjunction with infertility. Detailed results are provided in Table 2.
| Variables | Total Stigma | Self-stigma | Social Stigma | General Stigma | Family Stigma | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B (95% CI) | Robust S.E. | P-Value | B (95% CI) | Robust S.E. | P-Value | B (95% CI) | Robust S.E. | P-Value | B (95% CI) | Robust S.E. | P-Value | B (95% CI) | Robust S.E. | P-Value | |
| Age | |||||||||||||||
| 20 - 25 | Ref. | ||||||||||||||
| 26 - 30 | -4.3 (-10.2, 1.5) | 2.9 | 0.14 | 1.6 (-3.3, 0.17) | 0.90 | 0.07 | -0.5 (-1.9, 0.8) | 0.70 | 0.43 | -1.2 (-3.1, 0.7) | 1.01 | 0.22 | -1.1 (-3, 1.3) | 0.82 | 0.22 |
| 31 - 35 | -3.4 (-11.1, 4.7) | 4.0 | 0.40 | -1.6 (-3.7, 0.5) | 1.10 | 0.15 | -0.5 (-2.5, 1.4) | 0.99 | 0.57 | -0.7 (-0.9, 1.1) | 1.43 | 0.64 | -0.4 (-2, 1.8) | 1.02 | 0.70 |
| 36 - 40 | -5.3 (-7.3, 6.8) | 6.1 | 0.35 | -1.3 (-4.9, 2.2) | 1.82 | 0.47 | 0.3 (-1.2, 3.9) | 1.96 | 0.98 | -2.8 (-4.1, 2.3) | 1.82 | 0.13 | -1.2 (-4.2, 2.8) | 2.32 | 0.58 |
| Job | |||||||||||||||
| Housewife | Ref. | ||||||||||||||
| Employee | -5.0 (-9.3, 3) | 2.65 | 0.06 | -1.17 (-2.7, 0.4) | 0.77 | 0.134 | -1.3 (-2.5, -0.2) | 0.64 | 0.04 | -1.7 (-2.1, 2.3) | 0.96 | 0.07 | -0.8 (-1.5, 2.2) | 0.74 | 0.28 |
| Economic | |||||||||||||||
| Weak | Ref. | ||||||||||||||
| Relatively | -12.7 (-19.7, -4.3) | 8.64 | 0.14 | -3.8 (-8.8, 1.2) | 2.50 | 0.127 | -1.3 (-4.3, 1.8) | 1.58 | 0.1 | -4.7 (-6.2, 2.4) | 3.14 | 0.13 | -3 (-5.1, 1.7) | 2.32 | 0.2 |
| Rich | -21 (-23.7, -3.4) | 8.96 | 0.01 | -6.1 (-9.2, 0.9) | 2.60 | 0.20 | -2.9 (-3.2, 0.4) | 1.70 | 0.09 | -7.4 (-8.5, -3.2) | 3.28 | 0.02 | -4.7 (-6.4, -1.2) | 2.37 | 0.04 |
| Reason of infertility | |||||||||||||||
| Female | Ref. | ||||||||||||||
| Both | -0.09 (-0.02, 1.2) | 3.10 | 0.73 | -0.25 (-0.3, 1.2) | 0.90 | 0.77 | -0.4 (-0.8, 1) | 0.73 | 0.60 | 0.5 (-0.3, 2.4) | 1.05 | 0.60 | -0.8 (-2.3, 1.8) | 0.84 | 0.31 |
| Male | -31.9 (-33.2, 2.3) | 7.81 | 0.46 | -0.04 (-0.1, 2.2 | 1.04 | 0.96 | -0.4 (-1.1, 0.9) | 0.82 | 0.58 | -1.1 (-3.2, 2.7) | 1.19 | 0.33 | -0.9 (-2.4, 3.9) | 0.91 | 0.29 |
| Underlying disorder | |||||||||||||||
| Yes | Ref. | ||||||||||||||
| No | -107.1 (-120, -0.2) | 4.22 | 0.01 | -3.19 (-5, -0.2) | 1.21 | 0.009 | -1.5 (-2, 1.2) | 0.91 | 0.10 | -2.7 (-4, 2.8) | 1.44 | 0.06 | -2.6 (-4.1, -1.1) | 1.07 | 0.01 |
Multiple Linear Regression in Total Infertility Stigma and Its Components
5. Discussion
The present study aimed to identify the factors predicting stigma related to infertility. We reported women's perceptions of infertility stigma based on a median score, while a study conducted in Zahedan, Iran, utilized the mean score (24). Although a direct comparison of these scores was not feasible, it was observed that infertility stigma in that region was reported to be high. The population of Zahedan, located in the central Balochistan province of Iran, tends to favor larger families, a trend not observed in Tehran. Consequently, the stigma score was at a medium level in our study. Researchers suggest that the perception of infertility stigma varies based on a community's inclination towards childbearing (24).
In this context, a study conducted in Turkey in 2021 reported an average stigma score of 87.6 ± 27.9 among infertile women (25), indicating a high level of stigma in Turkey. However, the level of infertility stigma in the present study was lower than in the Turkish study. This discrepancy may be attributed to several factors. First, Iranian culture has evolved, with couples increasingly choosing to have only one or two children. Second, many couples are planning for pregnancy at a later stage in life. Third, access to artificial reproductive technology has improved, with advancements in conception assistance procedures. Overall, the birth rate in Iran has declined, which may have contributed to a reduced perception of infertility stigma; however, this issue warrants further research.
Previous studies have demonstrated that in communities with a strong preference for larger families, women who are unable to conceive often face significant stigma and subsequent social isolation (26, 27). For instance, a study conducted in Nigeria underscored the societal expectations placed on women regarding motherhood, highlighting the high reproductive expectations prevalent in Nigerian culture (28). Similarly, research has shown that women in Israel also encounter considerable infertility stigma (14). Additionally, investigations in Nigeria revealed that social expectations surrounding pregnancy within the cultural context can inflict psychological harm on infertile women grappling with the challenges of unsuccessful pregnancies (29).
In the present study, the age of women was not found to be associated with infertility stigma. A 2013 study conducted in Maine, USA, indicated that infertile women make pregnancy decisions based on their age. It was reported that younger women under 20 and older women over 40 experienced less infertility stigma when seeking assisted reproductive technology (ART), as societal expectations for pregnancy are comparatively lower in these age groups. Although motherhood and the desire for pregnancy and childbirth result from deliberate choices, women typically pursue childbearing at specific stages of their lives (30). The majority of participants in the present study were between 20 and 30 years old; however, their age did not exhibit a significant relationship with total stigma or any of the components of infertility stigma. Future research with a larger sample size may be warranted.
In this study, employment was found to be associated with some components of infertility stigma. The results indicated that employed women experienced lower perceptions of social stigma and public stigma compared to their unemployed counterparts. However, total stigma, family stigma, and self-stigma did not show an association with employment status. One study suggested that employment may help women feel less affected by infertility stigma and its consequences (7, 12). Janković and Todorović reported that some women perceive social capabilities, such as outside employment, as positively contributing to their self-perception, even in the context of infertility (31). Several factors may explain this phenomenon; employed women may be less concerned about the financial implications of infertility treatments, as financial stability enables them to cover such expenses. Moreover, community engagement may alleviate feelings of deprivation, thereby mitigating public perceptions and societal attitudes toward infertility.
The level of education among women did not correlate with perceptions of infertility stigma. A Japanese study supports these findings, reporting no relationship between education level and infertility stigma (8). Conversely, a Taiwanese study found that higher educational levels empower women, enabling infertile women to achieve greater self-sufficiency and manage negative emotions more effectively (32). While education level was not directly associated with infertility stigma, it appears to have an indirect influence on stigma. Educated women are likely to have better employment opportunities and greater economic support compared to those with lower levels of education. As noted by Logan et al., access to employment fosters a more equitable relationship dynamic between men and women in the community (33).
In the present study, the reasons for infertility were not found to be associated with the perception of infertility stigma. Factors related to female infertility, male infertility, or unknown causes did not correlate with stigma perception. However, based on our observations in Iranian culture, women experience infertility stigma even when the cause is male-related, often internalizing this stigma. One study indicated that infertile women in Tehran, Iran, with a history of female or unknown infertility causes experienced greater distress compared to those whose infertility was attributed to male factors (34). Additionally, research conducted in Africa reported a prevailing belief that women are solely responsible for infertility, with society rarely recognizing male infertility, attributing childlessness primarily to women (35).
Chronic conditions such as thyroid disorders, elevated prolactin levels, and obesity, which require treatment for these women, were linked to total stigma, self-stigma, and family stigma. These health issues appear to expose women to critical remarks and ridicule from acquaintances and family members. The results indicated no significant difference between general stigma and family stigma concerning these chronic diseases. Conversely, one study reported that most infertile women perceived family stigma due to their inability to conceive (36). It seems that disruptions in the reproductive system, such as issues with the uterus and ovaries — which symbolize femininity — play a more significant role in the perception of infertility stigma, while disturbances in other organs may not elicit such perceptions. In this context, one study suggested that infertile women suffering from conditions like polycystic ovary syndrome (PCOS), premature ovarian failure (37), premenstrual dysphoric disorder (38), or endometriosis (39) have an elevated perception of infertility stigma. However, the specific impact of each disorder on the perception of infertility stigma remains to be elucidated.
The study had several limitations. Firstly, it was conducted at a single infertility center. Although this center serves women from various cities, it is a public educational institution predominantly attended by individuals from similar economic and social backgrounds, which may influence the study's outcomes. In contrast, results from private or non-educational centers might differ. Therefore, future studies should be conducted in non-governmental and non-educational infertility centers to facilitate a more comprehensive comparison of perceptions of infertility stigma among women. Additionally, this study employed a cross-sectional design, limiting its ability to establish causal relationships; a case-control or cohort study would be more suitable for drawing definitive conclusions. Furthermore, qualitative research is essential to explore the deeper beliefs surrounding women's infertility, particularly to uncover the complex relationships between stigma and employment.
5.1. Conclusions
The findings of this study indicate that factors such as age, level of education, duration of marriage, duration of infertility, and reasons for infertility were not significantly related to the perception of infertility stigma. However, infertile women with unfavorable economic status experienced higher levels of infertility stigma. This highlights the need for targeted psychological counseling and financial support through expanded insurance coverage. Additionally, housewives who perceive higher infertility stigma should receive enhanced services and support. Women with comorbidities also reported elevated levels of infertility stigma, necessitating appropriate medical interventions. There is a pressing need to expand economic support and insurance coverage for infertility treatments within health policies. Furthermore, it is important to assess other factors not examined in the current study.