1. Background
In December 2019, several patients with pneumonia infected with the coronavirus were identified in a hospital in Wuhan, China, and their number was increasing daily (1). On January 9, 2019, China's Center for Disease Control and Prevention identified severe acute respiratory syndrome (SARS)-CoV-2 as the causative agent of Coronavirus disease 2019 (COVID-19) (2). This virus is among various viruses that cause mild colds, including Middle East respiratory syndrome (MERS) and SARS (3, 4). On January 30, 2020, the World Health Organization declared the COVID-19 epidemic a public health emergency of international concern (5).
The unknown epidemiological characteristics and transmission cycle of COVID-19 make it challenging to implement effective control policies (6). The interval between the onset of a person's symptoms and the identification of a second case of COVID-19 is about 4 to 5 days, which is considered the incubation period (7). The disease incubation period ranges from 2 to 11 days, with a maximum of 14 days. The World Health Organization has announced that the time between the onset of symptoms and death ranges from about 2 to 8 weeks (8).
Studies have shown that most transmission occurs near and before the appearance of symptoms (7, 9, 10). With early diagnosis, the risk of disease transmission decreases (11). The increase in undetected and untracked cases in the general population, which often lack clinical symptoms, leads to a rise in positive COVID-19 cases (12). According to Guan et al.'s study (as cited by Wang et al.), 50.5% of COVID-19 patients had chronic diseases, including cerebrovascular and cardiovascular diseases (13). In 32.2% of identified COVID-19 patients, at least one coexisting disease was reported, with the most common being hypertension (14.9%) and diabetes mellitus (7.4%) (14). According to the Chinese center for disease control (CDC)'s weekly report, hypertension is the most common underlying disease (12.8%), followed by diabetes mellitus (5.3%) and cardiovascular disease (4.2%) in COVID-19 patients (15). Due to the global spread of the COVID-19 in 2019, we will undoubtedly face an increase in the number of people infected with COVID-19 in autopsy cases. Although a history of fever and respiratory problems has been reported in some cases, epidemiological studies indicate that most people infected with COVID-19 experience mild or no symptoms, suggesting that approximately 40% of transmissions occur before symptoms appear. On the other hand, people who die from COVID-19 may still be infectious (12, 16).
Performing microbiological tests after death is necessary to rule out or confirm the presence of a COVID-19 infection. Forensic pathologists play a crucial role in addressing this by conducting autopsies during the COVID-19 pandemic, as the disease is relatively new and its causes are not yet fully understood (17, 18). Some of the potential roles of forensic medicine in this issue include determining the exact cause of death among those who tested positive for SARS-CoV-2, contributing to the accuracy of mortality statistics, understanding the pathological mechanisms of COVID-19, tracking the presence of the virus over time, and studying the survival of the virus after death (19). Furthermore, how long the virus persists or remains active in corpses is unknown (17).
In response to the COVID-19 pandemic, various countries have adopted specific diagnostic measures, including laboratory-based molecular tests. As stated by the WHO, a rapid test is one of the rapid diagnostic tests (Ag RDTs) used to identify cases of COVID-19, with a sensitivity of 80% and a specificity of 97%. Nevertheless, it should be noted that after the disease's acute stages, these Ag RDTs may increase the number of false-negative cases as the viral load decreases. Due to the limitations of molecular tests, including the relatively long period required to announce results compared to Ag RDTs, which leads to a delay in confirming or rejecting COVID-19 in individuals and makes monitoring and controlling the disease at both individual and social levels difficult, Ag RDTs are a suitable method for disease management and control (20, 21).
Despite being specific, these tests are less sensitive than molecular tests; however, when molecular tests are not available, and considering that these tests, despite being less sensitive than molecular tests, provide the possibility of a faster and more affordable diagnosis of SARS-CoV-2 in people with a high viral load, they are used for disease management and control. The use of Ag RDTs at the population level aims to identify individuals who are infectious or at risk of transmitting the infection (22). Additionally, this test identifies symptomatic and asymptomatic individuals with a viral load within the detection range of Ag RDTs, thereby preventing disease transmission to healthy individuals (23, 24). The positive predictive value of rapid tests is highly dependent on disease prevalence. The probability of testing positive when using Ag RDTs in asymptomatic individuals is estimated to be 1 - 2.5%, unless testing is performed in an area where COVID-19 is prevalent. The Ag RDT-positive results in this group should be confirmed with a specific Ag RDT or a molecular assay method to reduce the number of false-positive results (22). In the study by Castillo et al., 75.9% of the test results performed on corpses showed agreement between infectious disease diagnoses using complete diagnostic autopsy (invasive) and minimally invasive autopsy (rapid diagnosis) (25).
Coronaviruses typically remain outside the host for a few hours but can survive for several days under certain conditions. Human coronaviruses can survive on inanimate surfaces, such as metal, glass, and plastic, for 2 to 9 days (26) These viruses persist longer at a relative humidity of 50% than at 30% (27). Taking samples from corpses or preparing biological liquid swabs has been effective in controlling contagious diseases during outbreaks (28).
2. Objectives
The study aims to determine whether SARS-CoV-2 remains in corpses after death.
3. Methods
The present cross-sectional study examined the epidemiological status of deceased individuals referred to forensic medicine regarding COVID-19 infection, based on rapid diagnostic test (RDT) results from Zahedan, Khash, and Saravan cities in Sistan and Baluchistan province, Iran. All bodies referred to forensic medicine from March 21, 2021, to September 22, 2021, were included in the study. All positive or suspicious RDT cases were re-evaluated by PCR to confirm the diagnosis. Informed consent was obtained from the families of the study participants to perform the RDT test and, if necessary, PCR.
According to the study's purpose, all members of the research community, specifically all deceased individuals referred to forensic medicine, regardless of the cause of death recorded on the death certificate, were included in the study. In this study, the direct cause of death (not the individual's underlying diseases) was considered the cause. Based on the statistics of the deceased in previous years of forensic medicine, the expected sample size was 700 people; however, considering that the samples were included in the study through a census method, the number of deaths in the six months of the year was 810, and this number of samples was included in the study.
The tool for gathering information was a checklist created by the researcher, which was designed based on the variables needed to conduct the research (identity information and the test results of the deceased), and the necessary corrections were applied by obtaining the opinions of forensic medicine experts and experts from Zahedan University of Medical Sciences. Information related to the history of hospitalization, infection with COVID-19, and vaccination of individuals was collected through the medical care monitoring center (MCMC) system, the standard forms of the COVID-19 epidemic management and control plan notified by the Ministry of Health, and the university's written list of COVID-19 patients. To ensure the accuracy of the tests and prevent secondary contamination of the deceased by the samplers, weekly tests were performed on personnel working in forensic medicine who dealt with corpses. These individuals were prohibited from contacting the bodies if their test was positive.
A trained forensic expert used a sterile swab to collect body samples. A sample was taken from the deceased's nasopharynx and immediately tested using a RDT. If the test result was positive or suspicious, an additional sample from the deceased's nasopharynx was immediately prepared and sent to the University of Medical Sciences' reference laboratory for PCR testing. The PCR test was performed in RDT-positive cases because the test's positive predictive value was reported to be about 81% (29). Therefore, the possibility of a false positive result could not be ignored.
Some of the deceased may not have been referred to forensic medicine, for example, individuals who were hospitalized for a long time or those who died in villages and were buried immediately. Therefore, the possibility of selection bias in the study could not be ruled out and was considered a limitation of the study. Data analysis was performed using SPSS version 26 software. The chi-square statistic was used to compare the groups. The significance level of the statistical tests was set at 0.05. Zahedan University of Medical Sciences approved the research project with the ethical number IR.ZAUMS.REC.1400.093.
4. Results
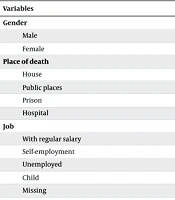
Of the 810 deceased cases referred to forensic medicine, 584 (72.1%) were men, and 226 (27.9%) were women. The average age was 39.5 years (ranging from 25 to 110 years), with a standard deviation of 22.9 years. Of all the deaths, 717 individuals had Iranian citizenship, and 92 were non-Iranian (Afghan and Pakistani). The highest number of deaths occurred at home, with 336 cases (41.5%), followed by deaths in public places (accidents, homeless individuals, etc.) with 332 cases (41%). Additionally, 113 individuals (14%) died in the hospital, and 29 individuals (3.6%) died in prison. Most of the deceased referred to forensic medicine (396 individuals, 48.9%) were illiterate. Among the deceased, 378 individuals (46.7%) had primary to high school education, and 27 individuals (3.3%) had a university education.
Moreover, 41 individuals (5.1%) were salary earners (employees, workers, or retired), 344 individuals (42.5%) were self-employed, 92 individuals (11.4%) were children, and 344 individuals (42.5%) were unemployed or housewives. In terms of place of residence, 657 individuals (81.1%) lived in the city, 128 individuals (15.8%) lived in the village, and 25 individuals (3.1%) were citizens of other countries or had an unknown residence status. Of all the deceased, 123 individuals (15.2%) had at least one crucial underlying disease, while 685 individuals (84.6%) did not have any specific history of underlying diseases. High blood pressure and cardiovascular diseases were the most frequent, reported in 90 cases (11.1%). This was followed by diabetes, reported in 12 cases (1.5%), and cancer, reported in 8 cases (1%). Other diseases were reported in 13 cases (1.6%).
Among all the deceased referred to forensic medicine, 17 individuals (1.2%) had a history of COVID-19 infection. The RDT test was positive for 30 individuals (3.7%) and suspicious for six individuals (0.7%) of all the deceased. All six suspicious RDT cases were confirmed after PCR testing. Additionally, all 30 RDT-positive cases were confirmed by PCR testing.
The highest rate of positive tests, 7%, was observed among individuals who died in the hospital, followed by those who died at home, with a rate of 6.8%. None of the individuals who died in prison tested positive. Among the deceased cases, 16 individuals (2%) had a history of hospitalization due to severe acute respiratory infection (SARI), of whom 13 cases (81.3%) had a positive test. Only 2.9% of the cases with no history of hospitalization tested positive.
Of the 17 cases that had a history of being infected with COVID-19 and were referred to forensic medicine after death, 12 cases (70.6%) had a positive test. Meanwhile, out of 769 cases without a history of COVID-19, 22 cases (2.9%) had a positive test after death (P < 0.001). No contact history was mentioned for 24 cases. Out of 810 deaths, only 4 cases (0.49%) had a history of contact with a COVID-19 patient, of which 2 cases (50%) had a positive test. Out of 89 cases of death due to SARI (at home or in the hospital), 28 individuals (31.5%) had a positive test. Meanwhile, only 5 cases (1.4%) of deaths caused by unintentional accidents, one case (0.8%) by intentional accidents, and one case (0.5%) with other diseases had a positive test result, with a P-value of less than 0.001.
Out of 631 individuals who were tested less than 24 hours after death, 29 individuals (4.6%) tested positive. Additionally, out of 128 cases that were sampled between 1 and 3 days after death, 3 individuals (2.3%) tested positive; out of 37 cases that were sampled between 3 and 7 days after death, 2 cases (5.4%) tested positive; and out of 14 cases that were sampled after 7 days of death, 2 individuals (14.3%) had a positive test (P = 0.153).
The average time interval between death and sampling among those who tested positive was 32.6 hours, while among those who tested negative, it was 31.9 hours (ranging from a minimum of 2 hours to a maximum of 240 hours). The average time interval between the last COVID-19 vaccination dose and death was 69.8 days in positive cases and 81.9 days in negative cases, with a P-value of 0.746.
Among the deceased with a history of receiving only one dose of the COVID-19 vaccine, the test results showed that 56 individuals (98.2%) were negative, and 1 individual (1.8%) was positive. Among the deceased with a history of receiving two vaccine doses, the test results showed that 87 individuals (96.7%) were negative, and 3 individuals (3.3%) were positive. Among the deceased without a history of receiving the vaccine, the results showed that 553 individuals (94.5%) were negative, and 32 individuals (5.5%) were positive. Among the eight deceased individuals who received three vaccine doses, none tested positive for COVID-19 (Table 1).
| Variables | COVID-19 Positive | COVID-19 Negative | Total (No.) | P-Value b |
|---|---|---|---|---|
| Gender | 0.261 | |||
| Male | 23 (3.9) | 561 (96.1) | 584 | |
| Female | 13 (5.8) | 213 (94.2) | 226 | |
| Place of death | 0.001 | |||
| House | 23 (6.8) | 313 (93.2) | 336 | |
| Public places | 5 (1.5) | 327 (98.5) | 332 | |
| Prison | 0 (0) | 29 (100) | 29 | |
| Hospital | 8 (7) | 105 (93) | 113 | |
| Job | 0.113 | |||
| With regular salary | 2 (4.9) | 39 (95.1) | 41 | |
| Self-employment | 14 (4.3) | 311 (95.7) | 325 | |
| Unemployed | 20 (5.8) | 325 (94.2) | 345 | |
| Child | 0 (0) | 92 (100) | 92 | |
| Missing | 0 (0) | 7 (100) | 7 | |
| SARI history | < 0.001 | |||
| Yes | 13 (81.3) | 3 (18.7) | 16 | |
| No | 23 (2.9) | 771 (97.1) | 794 | |
| COVID-19 history | < 0.001 | |||
| Yes | 12 (70.6) | 5 (29.4) | 17 | |
| No | 22 (2.9) | 747 (97.1) | 769 | |
| Missing | 2 (8.3) | 22 (91.7) | 24 | |
| Contact by COVID-19 | 0.002 | |||
| Yes | 2 (50) | 2 (50) | 4 | |
| No | 31 (4) | 750 (96) | 781 | |
| Missing | 3 (12) | 22 (88) | 25 | |
| Cause of death | < 0.001 | |||
| Unintentional injuries | 5 (1.4) | 341 (98.6) | 346 | |
| Intentional injuries | 1 (0.8) | 120 (99.2) | 121 | |
| Respiratory infection | 28 (31.4) | 61 (68.6) | 89 | |
| Other | 1 (0.5) | 195 (99.5) | 196 | |
| Death-test interval (h) | 0.153 | |||
| > 24 | 29 (4.6) | 602 (95.4) | 631 | |
| 24 - 72 | 3 (2.3) | 125 (97.7) | 128 | |
| 72 - 168 | 2 (5.4) | 35 (94.6) | 37 | |
| 168 < | 2 (14.3) | 12 (85.7) | 14 | |
| History of vaccination | 0.146 | |||
| Vaccinated | 4 (2.6) | 149 (97.4) | 153 | |
| Unvaccinated | 32 (5.5) | 555 (94.5) | 587 | |
| Vaccine dose | 0.771 | |||
| 0 | 32 (5.5) | 623 (94.5) | 655 | |
| 1 | 1 (1.8) | 56 (98.2) | 57 | |
| 2 | 3 (3.3) | 87 (96.7) | 90 | |
| 3 | 0 (0.0) | 8 (100) | 8 |
Comparison of Different Variables in Terms of Infection or Non-infection with Coronavirus Disease 2019 in the Deceased Referred to Forensic Medicine a
5. Discussion
In this study, 810 deceased individuals referred to forensic medicine over six months in 2021, regardless of the cause of death, were included.
In our study, the highest number of deaths occurred at home, with 336 cases (41.5%), followed by deaths in public places with 332 cases (41%). Additionally, 113 individuals (14%) died in a hospital, and 29 individuals (3.6%) died in prison. Out of the 16 cases that died due to COVID-19 with a history of hospitalization, 8 cases (56.3%) were discharged from the hospital with personal consent and were cared for at home. These individuals had an average of 9 days of hospitalization in the isolated and general wards of the hospital, and 6 individuals experienced respiratory distress during hospitalization. Among those who died in the hospital, 8 cases (7%) had a positive test, and among those who died at home, 23 cases (6.8%) had a positive test. Meanwhile, 8 individuals (34.8%) among those who died at home and had a positive test also reported a history of hospitalization.
The average interval between hospital discharge and death at home was 15.1 days (ranging from 1 to 35 days). It seems that the delay in timely hospital admission led to patients being in critical condition, increasing the severity of the disease and resulting in higher mortality (30, 31). A study by Birkmeyer et al. revealed that prompt medical interventions and early hospital presentation are associated with decreased rates of severe adverse outcomes and mortality in COVID-19 (32). None of the prisoners who died in prison had a positive test. Upon entering prison, all individuals were screened for COVID-19, and positive cases were immediately isolated and treated. Therefore, all deceased cases were identified and treated before death. However, environments with excessive crowding and limited access to healthcare, such as prisons, are prone to outbreaks of infectious diseases, underscoring the importance of heightened surveillance and preventive measures (33) Reports presented worldwide indicate that individuals with a history of COVID-19 can also become re-infected with the virus if exposed to cases of COVID-19 (29, 30). In this study, 12 cases (70.6%) of the 17 deceased individuals who had a history of contracting COVID-19 and were referred to forensic medicine after death tested positive. Meanwhile, out of 769 cases without a history of COVID-19, 24 cases (1.3%) tested positive after death (P < 0.001). This finding was consistent with the results of Singh et al., which demonstrated that viral mutations and variations in individual immune responses contribute to differences in reinfection rates and that a single infection does not confer complete immunity (34).
It seems that some individuals develop a false sense of security after contracting the disease and subsequently expose themselves to high-risk environments with high viral loads without observing protective measures (35). Conversely, the virus's genetic diversity and high mutation rate, particularly in individuals with immune system defects, create conditions that enable the virus to evade immune responses (36, 37). Among patients with SARI, 13 cases (81.3%) tested positive, while only 2.9% of those without a history of SARI tested positive (P < 0.001). According to epidemiological findings collected from 190 COVID-19 patients at the Policlinico Umberto I Hospital in Rome, 63.6% of patients reported an influenza-like illness (ILI) in their clinical history 1 to 3 weeks before the onset of symptoms associated with COVID-19. The ILI can be considered a risk factor for contracting SARS-CoV-2 in the future (38). According to the statements of the relatives of the deceased, out of 810 deceased cases, only 4 cases (0.49%) had a history of contact with a COVID-19 patient, of which 2 cases (50%) tested positive. It should be noted that, since the relatives of the deceased were asked about the deceased person's contact history, some relatives may not have been aware of the actual contact history. In the study by Chen et al., 44 individuals (12%) of the deceased had a history of close contact with people confirmed to be infected with COVID-19 (31).
In the study by Cheng et al., 5.5% of family contacts, 2.8% of non-family contacts, and 25.3% of individuals exposed through healthcare systems were infected with COVID-19 (39). In our study, the average time interval between death and sampling was 32.6 hours for those who tested positive and 31.9 hours for those who tested negative. No significant difference was observed in the time interval between death and sampling between the two groups (positive and negative test deaths) (P = 0.942). Factors such as viral load at the time of death and sampling conditions appear to be more decisive determinants in the test results.
In our study, the RDT result of 7 individuals (0.86%) among the deceased who died more than 24 hours earlier was positive, and among them, after more than a week of death, the test result of 2 individuals (0.25%) was reported positive. One case tested positive after 10 days, and the second case after 8.5 days postmortem. The results showed that after more than 7 days, the remains of virus particles could still be detected in corpses. However, there was no significant relationship between the time interval from death to testing and the result (P = 0.153). The identification of viral RNA/antigens in cadavers shows that SARS-CoV-2 RNA can be detected in various tissues of cadavers for an extended period after death, depending on environmental conditions. This may indicate the coronavirus's high resistance to unfavorable environmental conditions (40, 41). The persistence and infectivity of SARS-CoV-2 in corpses underscore the critical need for meticulous personal protective equipment (PPE) protocols among medical personnel (42). However, the detection of SARS-CoV-2 RNA within cadaveric tissues does not inherently equate to a risk of disease transmission from the deceased (43).
In the study by Zhou et al., the longest duration of virus shedding was reported as 37 days in recovered patients and until death in deceased individuals (44). Additionally, some studies have reported that the duration of virus shedding in patients ranges between 3 and 60 days (45). There is no evidence that the virus is transmitted through the movement of corpses; however, considering that in the current study traces of the virus were detected in corpses up to 10 days after death, it is possible for transmission to occur during contact with the corpse and exposure. Contaminated body fluids should be minimized by wearing PPE. It is necessary to use appropriate eye protection and masks during autopsies, particularly when procedures that generate aerosols are performed (46). Invasive autopsies, which require specialized personnel and advanced equipment, cannot be performed in areas with limited resources; therefore, in recent years, less invasive autopsies have been recommended (47, 48). The average interval between the last dose of the COVID-19 vaccine and the time of death was 66 days among cases with a positive outcome. In these cases, 1 individual (2.8%) had received a single dose, and 3 individuals (8.3%) had received two doses of the vaccine. Thirty-two individuals (88.9%) had no history of COVID-19 vaccination. None of the positive cases had a complete vaccination history (three doses). Although only 4 (2.6%) vaccinated individuals had a positive test result compared to 32 (5.5%) of the unvaccinated individuals, this difference was not statistically significant (P = 0.146).
In the study by Juthani et al., 172 (18%) of 969 hospitalized patients with COVID-19 had received at least one dose of the COVID-19 vaccine during hospitalization. Of these, 103 individuals received one dose, 15 received two doses, and 54 received three doses of the vaccine (complete vaccination) 14 days before the PCR test result was positive. Vaccination against COVID-19 effectively prevents infection with COVID-19 or hospitalization (49). Vaccination is increasingly considered the ideal intervention against infectious diseases (50). Coronavirus disease 2019 vaccines have played a crucial role in controlling the COVID-19 pandemic, particularly in reducing the incidence of severe cases and deaths caused by the disease (51). The availability of vaccines is a crucial factor in reducing the number of new infections. Factors such as low education level, female sex, young age, and low income levels can reduce individuals' willingness to get vaccinated (52, 53). In the present study, 48.9% of the participants were illiterate, 46.7% had a primary to high school education, and only 3.3% had a university education. Additionally, in this study, hypertension and cardiovascular diseases were the most frequent underlying conditions, affecting 90 individuals (11.1%), followed by diabetes in 12 individuals (1.5%) and cancer in 8 individuals (1%).
Thirteen individuals (1.6%) had other underlying diseases; among the 810 deaths referred to forensic medicine, 123 cases (15.2%) had at least one underlying disease. No significant relationship was found between the presence of an underlying disease and a positive test result for COVID-19 in deceased cases (P = 0.83). In two separate studies by Zhou et al. and Wichmann et al., cardiovascular diseases and high blood pressure were reported as the most common underlying diseases among the deceased (44, 54). Having a chronic disease increases the likelihood of death due to COVID-19 (28). In the historical cohort study conducted by Zhou et al., all patients over 18 years of age who were hospitalized with laboratory-confirmed COVID-19 at Jinyintan Hospital and Wuhan Lung Hospital (Wuhan, China) and had been discharged or died by January 31, 2020, had an average age of 56 years (range: 18 - 87 years). Of the 191 patients studied, 137 were discharged, and 54 died. Among these cases, 91 patients (48%) had at least one underlying disease. The most common underlying diseases were high blood pressure in 58 individuals (30%), diabetes in 36 individuals (19%), and coronary artery disease in 15 individuals (8%) (44).
In our study, information related to the underlying diseases of the deceased cases was collected from their relatives. Considering that the information provided by relatives about the deceased may have been incomplete, as well as the lack of access to the relatives of several deceased individuals — such as non-Iranians and homeless people — and the lack of response due to the psychological conditions of those around them, it seems that the prevalence of underlying diseases is lower than in the general population. According to the data from the national survey of risk factors of non-communicable diseases (STEPS) report of 2021 in Sistan and Baluchistan province, the prevalence of high blood pressure was 27.8% (24.9 - 30.7%), cardiovascular diseases 4% (2.8 - 5.2%), and diabetes 13.8% (10.6 - 17%), which differ from the prevalence of these diseases among the deaths referred to forensic medicine. Furthermore, this study is predicated on forensic medical data, which may not fully represent the broader population affected by COVID-19. The study by Tchicaya et al. demonstrated that geographical, social, and cultural disparities, coupled with variations in access to healthcare, result in differential levels of vulnerability across diverse communities (55). The inadequacies in COVID-19 mortality registration systems have led to incomplete documentation of causes of death during the pandemic. Factors such as insufficient testing, inaccurate recording, and the indirect impacts of socioeconomic determinants contribute to underreporting COVID-19 statistics and limit the generalizability of findings (56). Similarly, in the present study, the inaccessibility of data regarding specific demographics, including non-native populations, homeless individuals, and the effects of geographical and cultural variations, could potentially influence the study's findings.
Chen et al. studied 799 patients, including 274 confirmed moderate-to-severe or critically ill patients with COVID-19 who were admitted to Tongji Hospital. One hundred and thirteen of these patients died due to COVID-19, and 161 patients fully recovered and were discharged. The average age of the patients who died was 68 years, which was significantly older than that of the patients who recovered. The male gender was more prevalent among deceased patients (83 individuals; 73%) than among recovered patients (88 individuals; 55%). Overall, 71 (63%) of patients who died and 62 (39%) of those who recovered had at least one chronic disease. High blood pressure, cardiovascular disease, and cerebrovascular disease among the patients who died were observed in 54 (48%), 16 (14%), and 4 (4%) individuals, respectively, whereas among the recovered patients, these conditions were observed in 39 (24%), 7 (4%), and 0 (0%) individuals, respectively. The average time from the onset of symptoms to death in deceased patients was 16 days, and the average hospitalization time to death was 5 days. Chronic high blood pressure and other cardiovascular diseases were more common among deceased patients than among recovered patients (31). In the study by Huang et al., which was conducted on patients with laboratory-confirmed 2019-nCoV infection with positive RT-PCR, less than half of the patients had underlying diseases (32%), which were diabetes (20%), high blood pressure (15%), and cardiovascular diseases (15%), respectively (57). In the study by Wichmann et al., 12 cases of death with COVID-19 were autopsied between one and five days after death; the average age of the deceased was 73 years. All samples had underlying diseases. Coronary heart disease and asthma or chronic obstructive pulmonary disease (COPD) were the most common comorbidities (50% and 25%, respectively). Additionally, all deaths occurred in the hospital (54). The mortality rate of COPD patients with a severe form of COVID-19 (hospitalization) ranges from 1% to 62%. In COVID-19, for patients with respiratory diseases (asthma, chronic respiratory diseases, COPD, acute respiratory distress), the probability of death and adverse outcomes is higher. The likelihood of death among hospitalized patients with COVID-19 with an underlying disease was twice as high as that of individuals without an underlying disease (48).
5.1. Conclusions
Developing community awareness about the importance of timely and early referral to the special care department for high-risk populations is crucial. Due to the persistence of virus particles for more than a week in the deceased and the positive test results observed in this study, it is suggested that personnel working in forensic medicine and all individuals who deal with the deceased in any way during epidemics of infectious diseases use less invasive methods and employ appropriate PPE during autopsies and any actions performed on corpses.
Less invasive methods are safer for health personnel, especially in infectious disease settings, and can be easily performed by trained technicians. Performing a non-invasive autopsy (including blood and cerebrospinal fluid sampling and collecting tissue samples from organs using biopsy needles, followed by histological and microbiological analyses) is a reliable tool for determining the causes of death. Especially in areas where the occurrence of infectious diseases is high, it can be used for prioritization and health planning for the vulnerable populations of countries.