1. Background
The COVID-19 pandemic significantly impacted global healthcare, including surgical practices. Multiple waves and surges of the disease led to substantial changes in the allocation of hospital resources. Initially, a considerable portion of hospital beds was prioritized for acute respiratory cases, resulting in the suspension or cancellation of most elective and non-urgent surgeries (1). However, following the first surge and a better understanding of the disease’s pathophysiology, a variety of international and local protocols were developed to resume surgical activities at surgical care centers. Despite these efforts, completely eliminating the risk of perioperative infection remained challenging (2).
Although multiple reports on the effects of the pandemic on pediatric urology have been published, there is no consensus on preoperative screening for patients, particularly in ambulatory surgical centers (3, 4). Moreover, there is a notable gap in the literature regarding the status of Iranian pediatric urology during the pandemic, with limited existing studies. Additionally, special considerations are necessary for the pediatric population compared to adults. Routine swab tests may be difficult for the pediatric population to tolerate. Furthermore, children exhibit lower rates of severe COVID-19 disease, morbidity, and mortality compared to adults (5). Consequently, it is imperative to tailor preoperative screening protocols for pediatric procedures, accounting for their distinct physical, emotional, and behavioral conditions.
2. Objectives
The present study aims to evaluate the efficacy of a straightforward institutional preoperative screening method in predicting adverse outcomes associated with pediatric ambulatory urology procedures.
3. Methods
3.1. Study Design
This retrospective cross-sectional study aimed to assess the effectiveness of a preoperative screening method in mitigating the incidence of symptomatic viral infections and non-surgical complications during six distinct pandemic peaks in pediatric urology surgery within Iran. The study included all patients who underwent pediatric urology procedures from February 2020 to March 2023. During this period, Iran experienced six significant peaks, with the latest associated with a heightened hospitalization rate (6). Ethical approval for this study was granted by the Iran National Committee for Ethics in Biomedical Research (IR.SBMU.MSP.REC.1402.354).
3.2. Setting and Population
The study was conducted at a private pediatric ambulatory surgery center in Tehran, Iran, involving all eligible patients scheduled for outpatient pediatric urology surgical procedures. Prior to surgery, a comprehensive COVID-19 contact history and physical examination were conducted for the patients and their guardians. Laboratory tests, including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), were performed 24 hours before surgery. Normal levels for ESR and CRP were considered 0 - 10 mm/hour and 0 - 1 mg/L, respectively. As the normal range for leukocytes in infants varies with age, different levels of white blood cells were used for each age percentile (7). Upper respiratory tract infection (URTI) refers to a condition with irritation and inflammation of the upper airway due to an infectious cause, with no history of chronic obstructive pulmonary disease, emphysema, or chronic bronchitis (8). Patients without clinical or laboratory signs of COVID-19 respiratory infection were scheduled for surgery. Conversely, surgeries for symptomatic children or those with elevated ESR or CRP were deferred for 14 days, contingent upon becoming symptom-free. A polymerase chain reaction (PCR) test was conducted for these symptomatic patients just before the next preoperative visit. All surgeries were performed by a qualified consultant pediatric surgeon at an outpatient surgical care center. Patients were discharged within a maximum of 8 hours, provided no acute complications were observed (9). The range of urology surgical procedures included circumcision, orchiopexy, meatal stenosis repair, inguinal hernia, hydrocele, urethra repair, and chordee correction, among others. Anesthetic methods included general anesthesia, mild-to-moderate sedation, regional, and local anesthesia. Local anesthesia was administered using weight-adjusted instillation of 0.5% lidocaine.
3.3. Correlation to COVID-19 Peaks
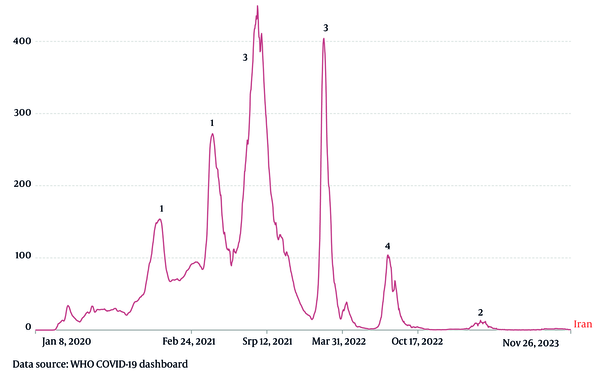
According to World Health Organization (WHO) statistics, COVID-19 had five major surges in Iran from February 2020 until March 2023, with one minor surge recently (Figure 1) (6, 10). The study measured the number of elective surgery cancellations during each COVID-19 surge and investigated the association between the surges and cancellations using analytical functions.
A graph illustrating the daily new confirmed COVID-19 cases per million individuals. The spikes indicate periods of increased cases. The Y-axis represents the daily number of positive tests nationwide, while the X-axis denotes the time period. Six notable peaks are identified, with numbers above each peak indicating the number of elective surgeries that were canceled during those times.
3.4. Data Gathering and Statistical Analysis
A medical field expert meticulously reviewed all medical records, entering the pertinent information into an electronic spreadsheet, which was then validated by a supervisor. Frequency and percentages were used for categorical variables, while central tendency functions (such as means and standard deviation) were utilized for continuous data. Additionally, chi-square analysis was employed to illustrate the association between surgery cancellations and COVID-19 spikes. The level of statistical significance for associations was set at 0.05.
4. Results
The study included 825 patients who were candidates for pediatric urology procedures during the pandemic, with a notable predominance of male patients (91.9% vs. 8.1%). The average patient age was 27.7 ± 30.0 months. As illustrated in Table 1, the most common procedures included circumcision, orchiopexy for undescended testis, meatotomy or meatoplasty, and inguinal hernia repairs. The preoperative questionnaire was completed by the children’s guardians, and initial laboratory tests were conducted as previously outlined. In total, 20 (2.4%) elective surgeries were either canceled or suspended due to patients’ clinical conditions or abnormal laboratory findings. High fever, cough, and URTIs, along with elevated ESR or CRP, were the leading causes of cancellation. Notably, only 2 (0.24%) patients with clinical symptoms of COVID-19 had a positive PCR result. Additionally, the number of cancellations during peaks five, four, and three was higher than during other peak surges. Fortunately, none of the patients developed COVID-19 in the postoperative follow-up period.
| Variables and Categories | No. (%) |
|---|---|
| Sex | |
| Male | 758 (91.9) |
| Female | 67 (8.1) |
| Age (mo) | |
| Mean ± SD | 27.7 ± 30.0 |
| Range | 1 - 203 |
| IQR | 27 |
| Procedures | |
| Circumcision | 247 (29.9) |
| Orchidopexy | 153 (18.5) |
| Meatotomy/meatoplasty | 147 (17.8) |
| Inguinal hernia a | 67 (8.1) |
| Hernia + hydrocele | 36 (4.4) |
| Urethral repair | 26 (3.2) |
| VUR b | 11 (1.3) |
| Other procedures c | 138 (16.7) |
Demographics of Patients who Underwent Pediatric Urology Procedures
4.1. Correlation with the Peaks
Out of the 20 children who exhibited preoperative symptoms, 14 subsequently developed COVID-19 symptoms during the identified peaks (Table 2). As represented in the table, the most frequent findings in patients whose surgery was canceled were fever, cough, and upper respiratory tract symptoms, followed by elevated ESR and CRP. Figure 1 illustrates the significant peaks of COVID-19 infection in Iran from the onset of the pandemic until the study date, with the corresponding number of symptomatic patients indicated next to each peak. Importantly, there exists a statistically significant correlation between preoperatively symptomatic patients and the occurrence of cancellations (P = 0.035).
Number of Elective Surgery Cancellation and Their Clinical and Laboratory Data
5. Discussion
The study findings reveal the landscape of pediatric urology procedures during the COVID-19 pandemic in Iran, providing crucial insights into the efficacy of the implemented preoperative screening method. The remarkably low rate of elective surgery cancellations (2.4%) indicates a successful mitigation strategy in balancing the maintenance of essential surgical services with safeguarding against COVID-19-related risks. Notably, the primary reasons for cancellations, including symptoms such as high fever and cough, underscore the importance of vigilant preoperative screening and contact history to prevent potential virus transmission within the surgical setting. Furthermore, the absence of postoperative COVID-19 cases, coupled with a low positivity rate in symptomatic patients, suggests a robust protective environment in the studied pediatric ambulatory surgery center. Additionally, the study demonstrated a significant increase in elective surgery cancellations during COVID-19 spikes.
Numerous studies have documented diverse approaches to preoperative screening prior to pediatric surgery. The most common methods include the SARS-CoV-2 RT-PCR test and strategies based on a combination of clinical and laboratory examinations. Each method presents distinct advantages and drawbacks. Research indicates that the preoperative PCR test may be controversial in both adults and children. While some studies report a high frequency of asymptomatic COVID-19 infection (detected by PCR), reaching up to 10% in certain centers (11), the majority of studies contend that the number of asymptomatic patients with positive PCR results is very low and negligible (12-15). Thus, in many tertiary centers, a widely adopted approach involves a combination of clinical and laboratory examinations for screening and scheduling elective surgeries. The use of PCR, while common, is not without its drawbacks.
Firstly, the PCR test is time-consuming and may cause delays in surgical scheduling. Additionally, the requirement for a nasopharyngeal swab, often necessary for PCR, can be challenging and discomforting, particularly for children. Moreover, PCR availability may be limited in low-income countries, potentially incurring additional costs for patients’ guardians, insurance companies, and national healthcare systems. Furthermore, the severity of COVID-19 infection in children is milder than in adults (16). With all this in mind, it seems reasonable to avoid routine preoperative PCR testing when planning elective surgeries, especially when resources are limited.
In the present study, there was a low rate of positive PCR results in symptomatic patients, and asymptomatic patients did not develop COVID-19 symptoms during a 14-day follow-up period. It is noteworthy that symptomatic patients were detected mostly during COVID-19 surges. Thus, extra care should be taken when scheduling patients during these peaks. Although several reports address the status of pediatric urology in different regions and countries, there is no specific study describing this issue in Iran (17-19). It appears that the current study is the only research dedicated to the status of pediatric urology in Iran.
Finally, there are special considerations regarding the setting of ambulatory and outpatient surgery compared to ordinary hospitalization in tertiary centers. First, ambulatory surgery centers only admit patients with elective surgical problems, while general pediatric hospitals admit COVID-19 cases. This may reduce the infection risk for patients undergoing elective surgeries (20). Secondly, operations in the outpatient setting are likely to be shorter and have lower general anesthesia rates (21, 22).
An important question that arises is, "Can we use our current experience with COVID-19 in potential upcoming outbreaks?" The answer is affirmative. As we know, SARS-CoV-2 caused one of the worst pandemics in terms of global health due to its extremely high transmission rate compared to other viruses. However, the fatality rate of the disease may be lower compared with other viral pandemics (23). Consequently, when pandemics are associated with viruses with high transmission and low fatality rates, these preoperative measures could be used to schedule elective surgeries. In cases of viral outbreaks with highly fatal viruses, caution must be exercised.
Although this report is the only one representing the status of preoperative pediatric urology screening in the setting of outpatient surgery in Iran, it does have some limitations. First, while it suggests that routine PCR testing for asymptomatic patients may be unnecessary, this could lead to missed cases of asymptomatic infections, raising questions about the utility of PCR testing. Additionally, the preoperative PCR test remains a controversial practice, indicating a lack of consensus in the medical community regarding its necessity. Although the study included a significant sample size of 825 patients, the low positivity rate in symptomatic patients (0.24%) may limit its ability to draw broader conclusions about screening effectiveness. Lastly, as a retrospective study, it may be subject to biases related to data collection and the accuracy of medical records.
5.1. Conclusions
Using a combination of clinical and laboratory examinations may suffice for preoperative screening of pediatric urology surgical procedures during the pandemic. Routine PCR testing is not recommended in this setting and should be confined to symptomatic patients. Moreover, the reported experience may be useful in addressing potential future viral outbreaks.